Online presentation Aug. 20, 2014

60 days of uncertainty:
Understanding the Affordable Care Act
90 Day Grace Period
This webinar is provided for discussion and informational purposes only.
Participants are encouraged to discuss the requirements and/or their obligations related to the Affordable Care Act with their attorneys or other advisors.
 About SCG Health
About SCG Health
The Searfoss Consulting Group, LLC opened in 2011 and is focused on revenue cycle management and strategic planning in this post-health reform world.
Services support the business of medicine with providers, associations, health plans and vendors.
Advocacy Communication & Engagement Education Provider satisfaction driver evaluation Strategic Planning
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Objectives
Objectives
Understand the 90 day grace period policy under the Affordable Care Act
Identify which patients the policy applies to and who it does not
Outline practical solutions to implement in your medical
practice to identify the patients and ways to mitigate retroactive denial
This webinar is provided for discussion and informational purposes only.
Participants are encouraged to discuss the requirements and/or their obligations related to the Affordable Care Act with their attorneys or other advisors.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
|
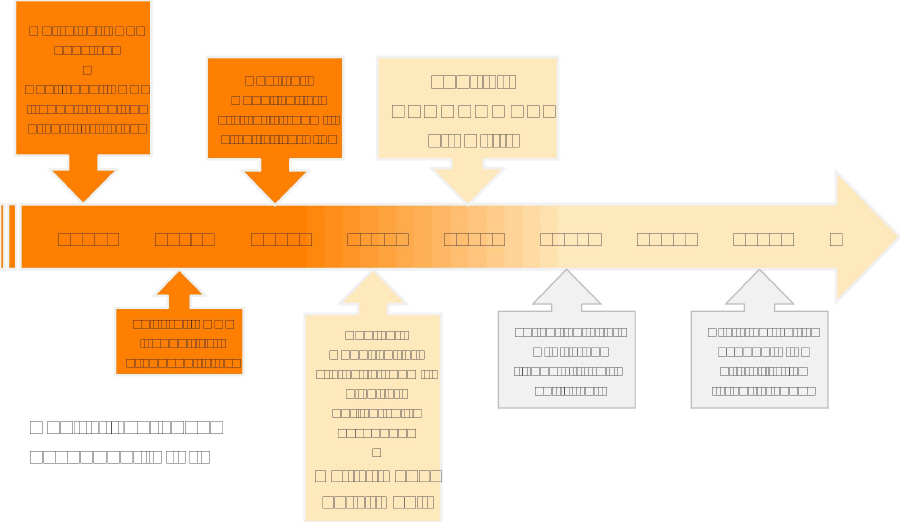
Timeline |
Open enrollment: October each year
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 ACA language
ACA language
P.L. 111-148, Section
1412
ADVANCE DETERMINATION AND PAYMENT OF
PREMIUM TAX CREDITS AND COST-SHARING REDUCTIONS
PAYMENT OF PREMIUM TAX CREDITS AND COST-
SHARING REDUCTIONS
(2)(B)(iv)(II) “allow a 3-month grace period
for
nonpayment of premiums before discontinuing coverage.”
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
|
Categories of beneficiaries |
||
HIX beneficiaries |
|
||
Federal subsidy = Advanced Premium |
insured and small business
policies where |
|
|
(b) qualified health plan product |
|
||
employer bears the risk. Insurance No subsidy = marketplace purchaser
companies only administer the network
and process claims. This falls under federal
jurisdiction. State law does not apply.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
What is the 90 day grace period 

Rulemaking finalized 7/15/2013 (on this provision)
45 C.F.R. § 156. 270(d)(3)
“(d) Grace period for recipients of advance payments of the premium tax credit.
“A QHP issuer must provide a grace period of three
consecutive months if an enrollee receiving advance payments of the premium tax credit has previously paid at least one full month's premium during the benefit year. During the grace period, the QHP issuer must:
“(1) Pay all appropriate claims for services rendered to the enrollee during the
first month of the grace period and may pend claims for services rendered to the enrollee in the second and third months of the grace period;
“(2) Notify HHS of such non-payment; and, “(3) Notify providers of the possibility for denied claims when an enrollee
is in the second and third months of the grace period.”
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 The policy in plain language
The policy in plain language
Applies to HIX beneficiaries
Must have received tax credit
Must have paid one month or more in premium
Health plan pays for services rendered during
first month of non-premium payment
Health plan must notify providers of possible
non-payment for services rendered between days 31-90 of premium non-payment
No standard on how notification is provided
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Practical implications
Practical implications
Member and provider
notice mandatory
For APTC beneficiaries, they
are to receive notice upon
delinquency (usually before
day 30) with pending grace
period end date. Once hit
day 31, information is
available to provider.
Patient education
necessary
As newly insured patients,
they may not understand the
importance of paying
premiums.
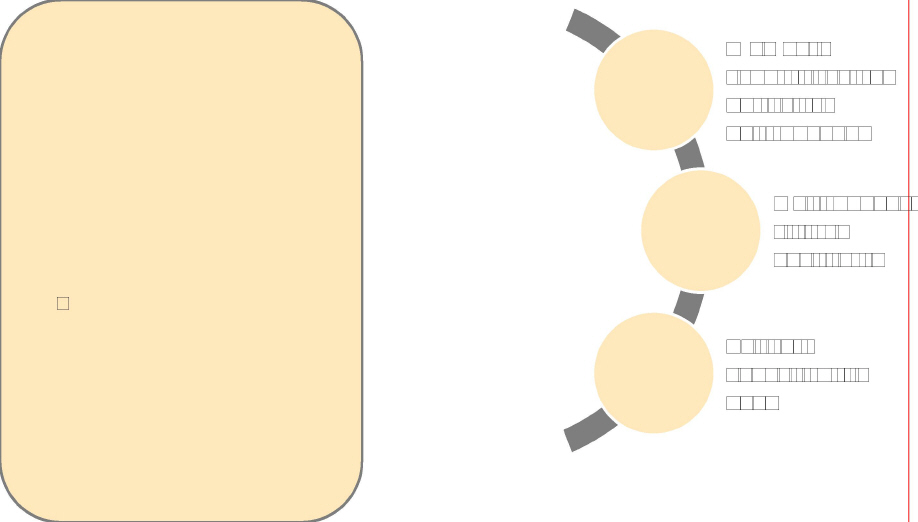
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 End-game
End-game
APTC delinquency premium is not paid within 90 days
Beneficiary liable for any provider charges during
period
Beneficiary liable to health plan for first month's
premium of grace period
Beneficiary liable to federal government for subsidy
Beneficiary is still on the hook for health
insurance and services
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
|
Reality by insured type |
|||
|
State law: |
|||
|
|
|
|
|
|
|
|
||
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
beneficiaries
APTC
Marketplace purchaser
beneficiaries
HIX
Non
 Best practices
Best practices
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
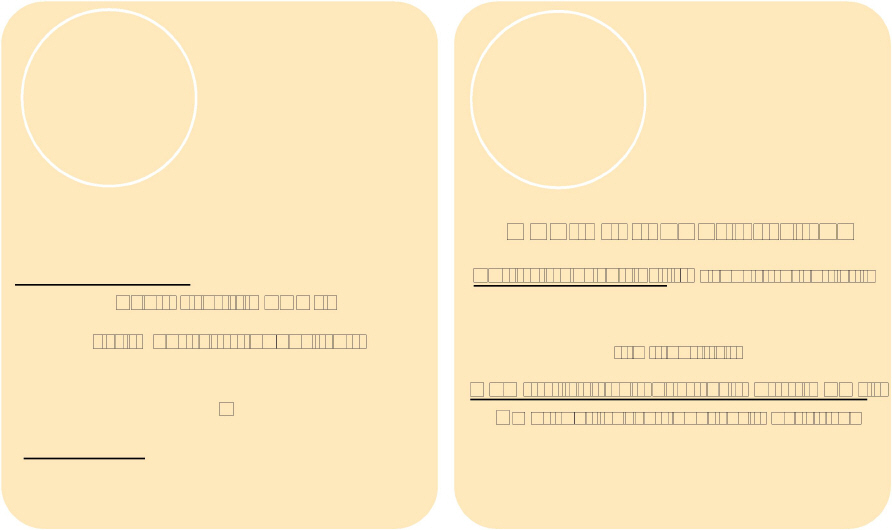
 Patient work flow
Patient work flow
Patient check-out
“Your balance due today is $75.45.
Patient intake
Would you like to pay by cash,
check or credit card?”
Remind patient of premium
payment status, payment
options, deductible and
copayment
Patient scheduling & reminders
Set the expectation of premium payment; service payment at time of service; tell patient their premium payment status, remaining deductible and copayment
Patient education What is their insurance? What is the
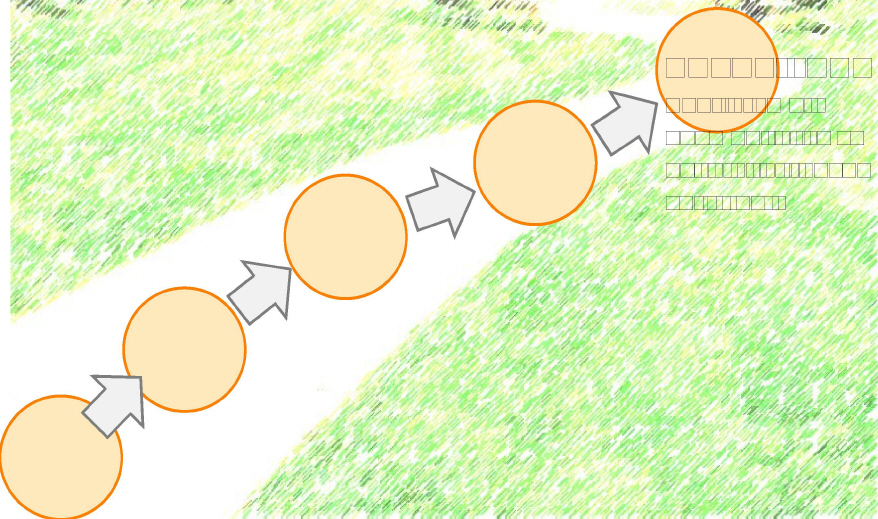
premium and what is coinsurance?
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
I (the patient) also understand and
acknowledge that I am personally
responsible to pay (the name of
the practice) in full for services that
my health insurer will not cover
due to non-payment of my health
insurance premiums.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
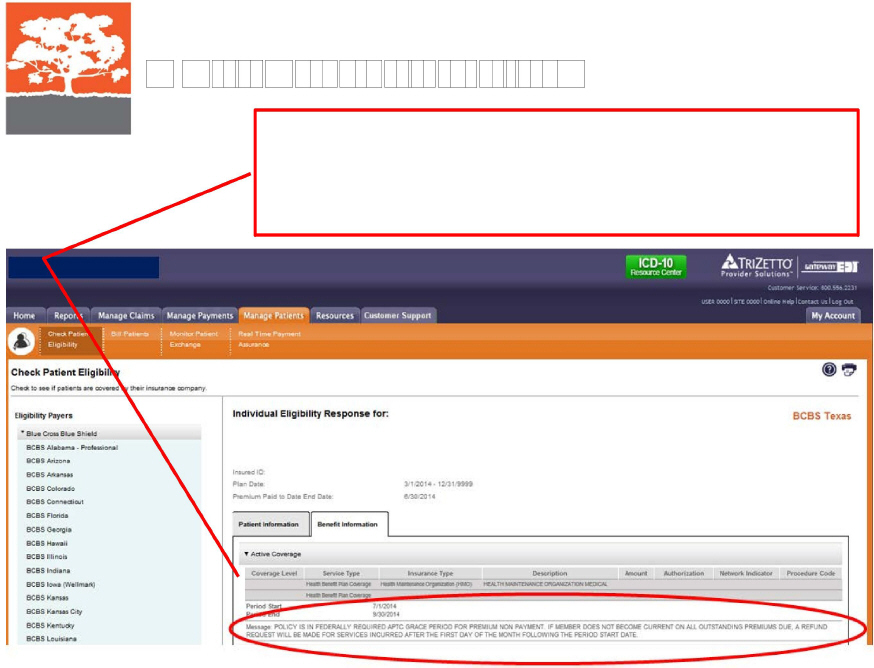
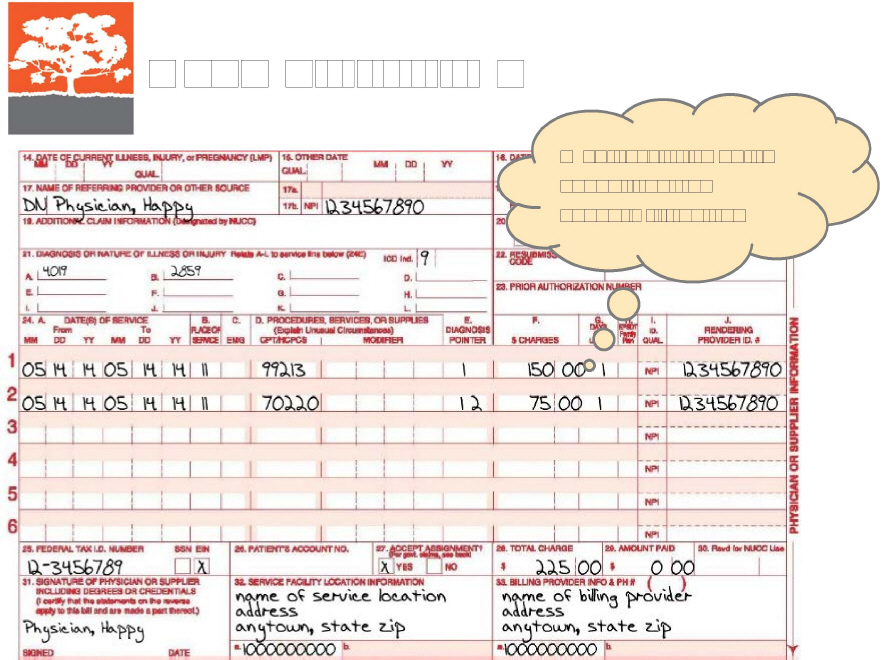
Message: POLICY IS IN FEDERALLY REQUIRED APTC GRACE PERIOD FOR PREMIUM NON PAYMENT. IF MEMBER DOES NOT BECOME CURRENT ON ALL OUTSTANDING PREMIUMS DUE, A REFUND REQUEST WILL BE MADE
FOR SERVICES INCURRED AFTER THE FIRST DAY OF THE MONTH
FOLLOWING THE PERIOD START DATE.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Validate eligibility/prior-auth
Validate eligibility/prior-auth
Electronic Phone Documentation
Document “Is this Copy of patient ID
card at each visit
account in Document Copy photo govt.
delinquency?” issued ID
Document

Date of inquiry
“When was Time of inquiry (can
the last pull call record)
Name of representative premium
Question asked and
paid?” answer provided
Staff training is essential for success!
Front office staff.
Back office staff.
Clinicians too.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Patient engagement
Patient engagement
Charges & self-pay
If patient is delinquent, then
they
are uninsured. What is your
policy? Generally, self-pay
rates will apply.
Best practices:
Claim shows charge rate
Once denial for delinquency
post-90 days, follow your
policy for patients in this
situation.
Be consistent!
For example: show the
charged and “discount” to
self-pay with full payment
expected within 30 days.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Premium payment assistance
Premium payment assistance
Interim final rule for Third Party Payment of Qualified Health Plan Premiums published on 3/14/2014
Both categories of HIX beneficiaries
Certain organizations may pay a portion or all of premium to
qualified health plans (FAQ clarification 2/7/2014) Ryan White HIV/AIDS programs
Indian tribes, tribal organizations and urban Indian organizations Private charitable
Qualified health plans do not have to accept (and are
encouraged to do so) premium payments made by hospitals, other health care providers and commercial entities
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
|
Example: self-pay |
|||||||
|
Service |
Medicare |
Charges |
Band |
Self-Pay |
Band |
|
|
|
99213 |
$73.08 |
$150.00 |
Double |
$110.00 |
Quarter |
|
|
|
70220 |
$39.76 |
$75.00 |
Double |
$60.00 |
Quarter |
|
|
|
If a patient can't
pay their premium due to financial need, how do you know? |
|||||||
|
Establish your policy for all patients that change insurance status |
|
||||||
|
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com. |
|||||||

 Discounting policy
Discounting policy
In clear terms, the government reiterated that federal law does not prohibit Medicare, Medicaid and state children's health insurance programs (SCHIP) providers from discounting services to the uninsured.
The government, however, remains Applicable laws
The Medicare Exclusion
suspect of waiver and discount Statute civil only
policies that fail to determine a
The federal Civil Monetary
patient's financial need. Penalty Law civil only
The federal Anti-kickback
Statute criminal only
The federal Stark Law
civil or criminal
The federal False Claims
Act civil or criminal
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
The government provides
review
basis. even for the same patient.
|
no universal definition
of
Special fraud alert
states that
|
|
return or pay stub. |
||
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
|
Checklist of key
policy |
||
In writing!!! |
Consistency across all payer types |
Establishes period
for documentation confidentiality policy |
|
What to ask for from patients: Copy of the latest W2, tax return, pay
stub, bank statement, etc. Were you considered for the Medicaid
program? You may request copy of Medicaid denial letter. Could you
accept a payment plan?
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Your homework
Your homework
Review intake procedures.
Is the front desk able to identify patients? |
|
Are patients aware of their premium
payment status |
|
Are you running and documenting
eligibility for every |
|
|
|
How does your software identify
claims for these |
|
Review your policies.
Know your resources.
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.
 Resources
Resources
American Medical Association
http://www.ama-assn.org/ama/pub/ advocacy/topics/affordable-care-act/ aca-grace-period.page
Medical Group Management
Association
State Medical Societies
All rights reserved. 2013-14 Searfoss Consulting Group, LLC. To distribute or copy, please contact jen@SCGhealth.com.