
Intellect™
BILLING MENU OPTIONS

View Claim Files
View Claim Files
This menu option is used to help track billing when bills are submitted using the Group of Patients option.
1. To open the View Claims Files screen in Intellect, select Billing --►View Claim Files:
The View CLAIM_FILES screen opens:
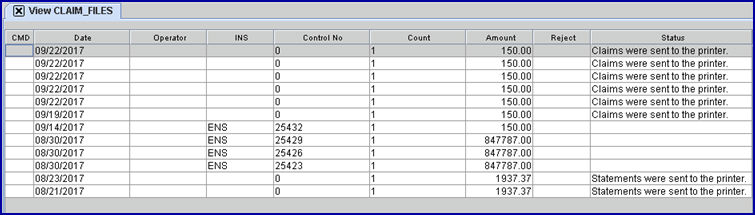
Effective version 9.12.31, the View Claim Files screen displays in descending date order and only includes the files generated in the last 90 days.
2. CMD ![]()
2.1 This field allows input for electronic billing only. Press [F2] to display three options:
V: Displays the way the claim file went to the clearinghouse.
9: This references a 997 report. A 997 report is only available if billing was done directly with an insurance carrier such as Medicare and not through a clearinghouse. When viewing the 997 report, if there is an 'A' on the line beginning with AK9, everything went through, and the word ACCEPTED displays in the Status column on the screen. An 'R' displayed on the line beginning with AK9 indicated something was rejected in the billing, and the word REJECTED displays in the Status column on the screen.
A: Displays an Acknowledgement Report if a report is available (if no Acknowledgement Report is available, an error message is displayed). After viewing the Acknowledgement Report, it can be closed three ways: 1) Click on the Close button at the bottom of the screen, 2) Click on the X in the top right corner of the screen, or 3) Press [ESC].
3. Date ![]()
3.1 The date the billing task ran.
4. Operator ![]()
4.1 Displays the Operator who submitted the bill for the claim.
5. INS ![]()
5.1 Indicates the insurance company to which the claim was billed. Prime Clinical commonly uses abbreviations such as MCAL for MediCal, but insurance identifiers vary based on how they are set up by individual clients.
6.1 Displays a control number generated by Prime Clinical for the group of patients' bills being submitted.
7. Count ![]()
7.1 The number of bills submitted.
8. Amount ![]()
8.1 The total dollar amount of the group of bills submitted.
Note: If a bill is transmitted electronically and there is a number in both the Control No. and Count columns but there is a zero in the Amount column, the transmission either failed or the clearinghouse has not yet processed the submission.
9. Reject ![]()
9.1 If the claim was rejected, a message displays in this column. If there is a message in this column, please call Prime Clinical.
10. Status ![]()
10.1 Indicates the status of the submitted bill(s).
10.2 If there is nothing displayed in the Status column, the clearinghouse or insurance company did not include the control number (see <Control No> above) in their report.
10.3 Status messages are:
• Claims were sent to printer: Displays when printing paper claims.
• Statements were sent to the printer: Displays when printing patient statements to paper.
• ACCEPTED: Displays when everything went through on an electronically submitted group of bills. This is displayed in conjunction with a 997 report. A 997 report is only available if billing was done directly with an insurance carrier such as Medicare and not through a clearinghouse.
• REJECTED: Displays when there was an error with an electronically submitted group of bills. This is displayed in conjunction with a 997 report. A 997 report is only available if billing was done directly with an insurance carrier such as Medicare and not through a clearinghouse. If this message displays, please call Prime Clinical.
• ELIGIBILITY SENT: Displays when an electronic billing transmission has been sent but there has not been a response from either the clearinghouse or the insurance company.