
Intellect™
CHARGES MENU OPTIONS

Vision Encounter
This menu option is used to post additional claim information needed to process a patient’s claim for vision-related claims. Use this form for electronic billing when Utility --►Procedure <Status> = 'V.'
See details on adding vision encounter information to a patient’s account in Intellect.
Updates:
Effective version 16.05.20
In prior versions, for the Internal Control Number (ICN) to be included in the Electronic Claims, the ICN had to be entered in the <Internal Control> field. Effective this version, Intellect now pulls the ICN number from the charge. This is handled by Intellect when auto-posting is used to post payments from the payers. This modification is NOT retroactive. Additionally, this ICN now also prints on the printer EOB from Intellect.
Effective version 14.07.01
When Intellect looks for a Referring Provider (a.k.a. ordering physician), Intellect first looks at the encounter screen for either <Ordering Provider> or <Supervising Provider> and, when either is blank, Intellect looks at the Utility --►Set Up --►Parameter <Referring> setting and pulls the referring provider based on the setting.
Effective Version 9.12.27
For clients who complete most of the Encounter screen fields with the same values for each patient, version 9.12.27 allows a 'default' record to be set up with the value to be carried over to all new Encounters.
To set up a default screen, go to Charges --►Encounter. Select the type of Encounter screen the office uses (the sample below is for Generic Encounter), then select Modify. At the <Patient Account No> field, enter 0 (zero). At the <Encounter #> field, enter 0 (zero).

Complete any field to default to all new Encounters entered.
Setting up the default encounter screen does NOT affect any encounters already entered.
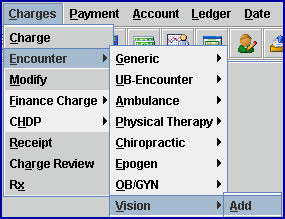
1. To add vision encounter information to a patient’s account in Intellect, go to Charges --► Encounter --►Vision --►Add
The Add Vision screen displays:
2. Patient’s Account No 
2.1 When not already displayed, type the patient’s account number, OR type up to 6 characters of the last name and press the [F2] key. To select the code from the list, either highlight the record and press the [Enter] key, OR double-click on the record.
3. Patients Name 
3.1 The patient’s name is displayed. This is a read-only field and may not be modified.
3.2 This field is formatted Last, First.
4. Encounter # 
4.1 This number is assigned automatically when adding a new record.
4.2 This number is used to individually display this encounter.
5.1 Type the authorization number given by insurer for this treatment.
5.2 Intellect completes Box 23 on the CMS 1500 form with this number.
Or, when used for electronic claims submission, Loop 2300 REF*G*1.
6. Encounter Description 
6.1 Type a meaningful description for this encounter.
7. Injury Date 
7.1 Type the date of injury for a Workers’ Comp case.
7.2 Effective version 14.09.29: This field is no longer required if the <DOI> field on the Registration --►Worker --►Worker Insurance screen is completed, since Intellect pulls the date from that field to complete the CMS 1500 or electronic equivalent.
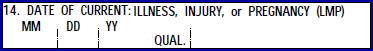
7.3 Effective version 13.12.12: For Workers’ Comp patients only (Utility --►Category <Type> = ‘W’ or ‘F’), Intellect completes Box 14 on the CMS form with the date and qualifier 439.
Or, when used for electronic claims submission, it is added to Loop 2400 DTP*439*
8.1 This is required on vision claims/encounters involving replacement lenses or frames. It specifies the Category to which <Condition Indicator 1> applies.
8.2 It uses electronic claims submission Loop 2300 CRC01.
8.3 Press the [F2] key to display the valid options and double-click on an option:
9. Certification Condition Indicator 1 
9.1 This indicates whether or not <Condition Indicator 1> applies. A 'Y' value indicates the condition codes in Loop 2300 CRC03 through CRC07 apply; an 'N' value indicates the condition codes in CRC03 through CRC07 do not apply.
10.1 Select the code indicating the reason for lens replacement.
10.2 It uses electronic claims submission Loop 2300 CRC03.
10.3 Press the [F2] key to display the valid options and double-click on an option:
11. Code Category 2 
11.1 This is required on vision claims/encounters involving replacement lenses or frames. It specifies the Category to which <Condition Indicator 2> applies.
11.2 It uses electronic claims submission Loop 2300 CRC01.
11.3 Press the [F2] key to display the valid options and double-click on an option:
12. Certification Condition Indicator 2 
12.1 This indicates whether or not <Condition Indicator 2> applies. A 'Y' value indicates the condition codes in Loop 2300 CRC03 through CRC07 apply; an 'N' value indicates the condition codes in CRC03 through CRC07 do not apply.
13.1 Select the code indicating the reason for lens replacement.
13.2 It uses electronic claims submission Loop 2300 CRC04.
13.3 Press the [F2] key to display the valid options and double-click on an option:
14. Code Category 3 
14.1 This is required on vision claims/encounters involving replacement lenses or frames. It specifies the Category to which <Condition Indicator 3> applies.
14.2 It uses electronic claims submission Loop 2300 CRC01.
14.3 Press the [F2] key to display the valid options and double-click on an option:
15. Certification Condition Indicator 3 
15.1 This indicates whether or not <Condition Indicator 3> applies. A 'Y' value indicates the condition codes in Loop 2300 CRC03 through CRC07 apply; an 'N' value indicates the condition codes in CRC03 through CRC07 do not apply.
16.1 Select the code indicating the reason for lens replacement.
16.2 It uses electronic claims submission Loop 2300 CRC05.
16.3 Press the [F2] key to display the valid options and double-click on an option:
17.1 This field is used as the date lenses were received or sent to the patient.
17.2 It uses electronic claims submission “DATE SHIPPED” Loop 2300 DTP 011.
18.1 This is required on claims where a prescription has been written for hearing devices or vision frames and lenses and it is being billed on this claim.
18.2 Effective version 13.12.12: Intellect completes Box 15 with the date and qualifier 471.
Or, when used for electronic claims submission, Loop 2300 DTP*471*D8
19.1 This field is used for electronic transmission if a particular claim is being transmitted in response to a request for information (e.g., a 277), and the response has been delayed. Loop 2300 CLM20.
19.2 To view the list of codes with descriptions press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
20.1 This field is used to designate a supplemental report type that is forwarded separately. It works with the <Report Transmission Code> and <Identification Code> fields. It uses electronic claims submission Loop 2300 PWK01.
20.2 To view the list of codes with descriptions press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.

21.1 This field is used to designate a supplemental report type that is forwarded separately. It works with the <Report Type Code> and <Identification Code> fields. It uses electronic claims submission Loop 2300 PWK02.
21.2 To view the list of codes with descriptions press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
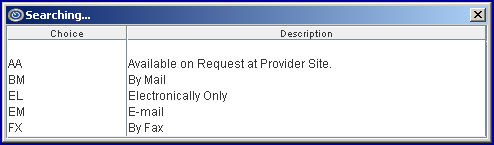
22.1 This field is used for electronic billing. Electronic claims submission Loop 2300 PWK06.
22.2 Type the Attachment Control Number from the pre-printed MEDI-CAL CLAIM Attachment Control Form. The form must accompany the supporting documentation.
NOTE: When completing the encounter record: it is recommended to include the ATTACHMENT CONTROL NUMBER as part of the Encounter Description.
22.3 PCM users only. Effective version 14.07.01:
22.3.1 With the focus in this field, press the [F2] key twice to display a list of document files pulled from the Progress Notes in PCM (the list does NOT include files generated in Intellect or manually saved to the /home/staff/EB_ATTACHMENT folder).
22.3.2 To display only a certain type of file, enter the beginning letters of the file and then press [F2].
22.3.3 Click on the appropriate file to select it. To select multiple files, hold down the [Ctrl] and [Shift] keys while clicking on the desired files. The file's Document Id displays.
23.1 The Claim Frequency Code is used only for electronic billing and indicates what type of claim it is. For example, an original submission, corrected claim which is being resubmitted, a replacement claim, or a voided claim. The default is set to 1: Original Submission. Prior to adding this field on the Encounter screen the system submitted all claims with Claim Frequency Code 1. Loop 2300 CLM05 - 3.
23.2 To view the list of codes with descriptions press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
23.3 When making an appeal for a Worker's Comp claim, in addition to this field, the <Internal Control>, <Appeal Type>, and <Appeal Documentation File> fields MUST be filled.
23.4 Effective version 18.08.31: When this field is set greater than 1 and the <Internal Control> field is blank, the ICN # that comes with the ERA file is printed in Box 22 on the HCFA 1500 and also sent electronically.
24.1 Enter the unique identification number assigned by the pharmacy or supplier to the prescription. It uses Loop 2410 REF02 with the Qualifier XZ.
25.1 EDS assigns each claim an Internal Control Number (ICN) systematically when it is received electronically or by mail. Processing or returning the claim constitutes EDS’ final action on that claim. A resubmission of the same service is considered a new claim. Each claim sent to EDS is assigned an ICN automatically, which is used to track the claim. The ICN is made up of 13 digits in a specific format. The format of the ICN enables the determination of when the EDS actually received the claim.
25.2 This field is used when rebilling a corrected claim to provide the insurance the original claim control number on a denied claim.
25.3 This number is included in the electronic transmission for all claims. It is a number assigned by the payer to identify a claim. The number is usually referred to as an Internal Control Number (ICN), Claim Control Number (CCN), or a Document Control Number (DCN). CLM, 2300 REF02 is the Loop and segment:
CLM*1.608.1.491.G*250***11:B:7*Y*A*Y*Y*P
REF*F8*20024E011000 ß
25.4 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Appeal Type>, and <Appeal Documentation File> fields MUST be filled.
25.5 Effective version 18.08.31: When this field is blank and the <Claim Frequency Code> field is set greater than 1, the ICN # that comes with the ERA file is printed in Box 22 on the HCFA 1500 and also sent electronically.
26.1 This field is used to identify the level of the appeal, if needed.
26.2 Use the drop-down list and select the appropriate option:
26.3 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Internal Control>, and <Appeal Documentation File> fields MUST be filled.
27.1 If there is documentation that needs to be sent to the insurance company, enter the file name of the documentation.
27.2 Files with valid file names are sent directly to the insurance company.
27.3 Effective version 14.07.01:
Clients with Intellect only:
27.3.1 Create and save Appeal Document(s) files in the /home/staff/EB_ATTACHMENT folder. SBRs may also be saved as a .pdf to the /home/staff/EB_ATTACHMENT folder and attached as appeal documents.
27.3.2 Type the exact file name in this field. Note: This field is case-sensitive.
Clients with both Intellect and Patient Chart Manager (PCM) only:
27.3.3 With the focus in this field, press the [F2] key twice to display a list of document files pulled from the Progress Notes in PCM (the list does NOT include files generated in Intellect or manually saved to the /home/staff/EB_ATTACHMENT folder).
27.3.4 To display only a certain type of file, enter the beginning letters of the file and then press [F2].
27.3.5 Click on the appropriate file to select it. Multiple files may be selected by holding down the [Ctrl] and [Shift] keys while clicking on the desired files. The file's Document Id displays.
27.4 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Internal Control>, and <Appeal Type> fields MUST be filled.
28. When the information is completely entered, select one of these options:

28.1 Click [Add] to clear the screen and return the focus to <Patient Account No>, saving the new encounter.
28.2 Click [Clear] to display this message:

28.2.1 Click [Yes] to clear the screen and return the focus to the <Patient Account No> field, saving the new encounter.
28.2.2 Click [No] to clear the screen and return the focus to the <Patient Account No> field without saving.
28.3 Click [Exit] to display this message:

28.3.1 Click [Yes] to clear the screen and return the focus to the main Intellect screen, saving the new encounter.
28.3.2 Click [No] to clear the screen and return the focus to the main Intellect screen without saving.