Intellect™
ERROR SUMMARY REPORT

Offices receive one Error Summary Report for each business day that they transmit claims to CABBS successfully, even if they transmit several times per day. If error messages appear on their report, they should refer to the 'Pre-pass Edits' list.'
Reading the Error Summary Report
The Error Summary Report contains three sections. The first section shows the total number of batches and claims, total charges per batch, and total dollar amounts for all batches accepted and/or rejected. The Internal Control Numbers (ICN's) assigned to the accepted claims are also displayed.
1. The Provider Summary section lists claim acceptance / rejections for individual providers. This section is especially helpful to submitters who send claims for multiple providers (or multiple groups) within the same file transmission.
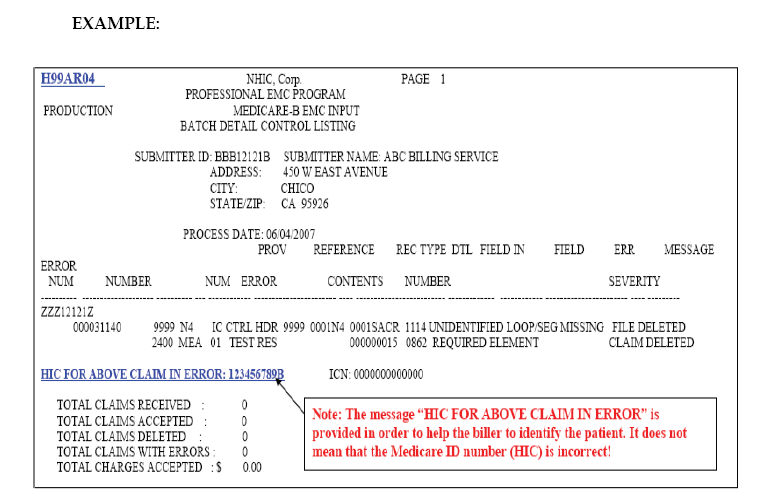
2. Batch Detail Control Listing: Batch Detail Control Listing shows all errors at the claim, batch, or file level. If a claim, batch, or file has been rejected, one or more error codes appear.
Each error code has a text message explaining the error. More detailed information is available in the 'Pre-pass Edits' lists. Batch level errors are identified by PIN/PTAN, NPI, and by batch number. Files, batches, or claims.
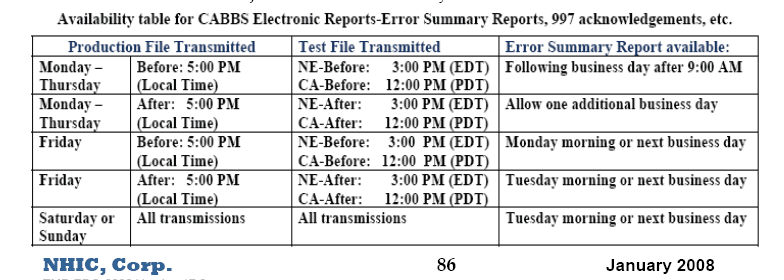
In addition to the information noted on the previous page, the Batch Detail Control Listing provides a summary of accepted and deleted claims at the batch level, at the file level, and at the 'submitter' level. The 'submitter' level includes all files received from the submitter for that report’s process date. Files received by CABBS after 5:00 p.m. (local time) are included on the Error Summary Report for the next business day.
3. The Summary Of Error Messages section lists all pre-pass edit messages and the number of times each edit failed for all providers within the report. Submitters can easily identify potential billing problems with this information.
If any claim, batch, or file has been rejected, one or more error codes appear on the Error Summary Report. Each error code has a brief text message explaining the error. Information that is more detailed is available in the 'Pre-pass Edit' list. Files, batches, or claims that are rejected at the pre-pass level need to be corrected and re-transmitted.
When used thoroughly and consistently, the Error Summary Report is a powerful tool that helps offices precisely track claims acceptance status while giving them the information they need to be able to correct and retransmit rejected claims immediately with no loss of cash flow.
NHIC, Corp. guarantees same-day acceptance for claim files that have been processed by the CABBS Claim Editor by 5:00 p.m. unless unforeseen circumstances occur, (natural disaster, power failure, etc.). Claims received after 5:00 p.m. are counted as received the next business day.
The Error Summary Report is posted to the office's CABBS electronic mailbox sometime between 9:00 a.m. and 12:00 p.m. It remains there for 15 calendar days. The report may be downloaded to an office computer for reformatting and printing. Offices should not delete Transmission Logs, Error Summary Reports, or ANSI 997’s from their mailbox unless they are certain they are no longer needed. Because each electronic mail message is automatically deleted from the CABBS after 15 calendar days, it is not necessary to 'clean out' the mailbox.
Do not delete Error Summary Reports (or ANSI 997s) from the office CABBS mailbox unless it is certain they are no longer needed. Mail deleted from the office mailbox may not be recoverable. CABBS automatically deletes any mail item after 30 calendar days whether it has been read or not. Please maintain copies of the error summary reports and/or ANSI 997 reports which show errors until the claim has been loaded successfully to CABBS.
This final summary shows all errors for all providers along with a count of how many times each error occurred in the file. This information may be used to quickly identify problem-billing areas. Use the ESR to help track claims acceptance status with precision and find the needed information to correct and re-transmit rejected claims immediately, with no loss of cash flow.