
Intellect™
CHARGES MENU OPTIONS

Specialty Charges
NDC Set Up/Billing via Paper & Electronically
and
BILLING MENU OPTIONS

Insurance
Paper Claim Resources
NDC Set Up/Billing via Paper & Electronically
Effective April 1, 2009, Medicaid and other insurance carriers began requiring NDC information for both paper and electronic billing. NDC information may be billed for both Professional and Institutional billing.
The Deficit Reduction Act (DRA) of 2005 required State Medicaid agencies to provide for the collection of NDCs on all claims for certain physician-administered drugs for the purpose of billing manufacturers for Medicaid drug rebates.
A physician-administered drug includes any covered outpatient drug provided or administered to a recipient, which is billed by a provider other than a pharmacy. Such providers would include, but not be limited to, physician offices, clinics, and hospitals. A covered outpatient drug is broadly defined as a drug that may be dispensed only upon prescription and is approved for safety and effectiveness as a prescription drug under the Federal Food, Drug and Cosmetic Act. Physician-administered drugs are not restricted to injectable drugs only. Physician-administered drugs include any drug regardless of the method of administration.
Such claims need to include NDCs, corresponding quantity amounts, Unit of Measure, and a prescription number for physician-administered drugs.
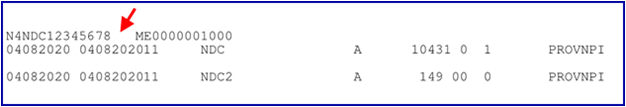
Effective version 21.01.27, when printing claims on HCFA 1500 forms that include an NDC number, the NDC now has 3 spaces between the NDC number and the QTY:
Your system must be set up as follows for appropriate physician-administered drugs for Medicaid, paper, and electronic claims submission. See additional information for paper claims.
Set Up:
Set up is completed on three screens:
1. Utility --►Procedure --►Procedure
1. Utility --►Procedure --►Procedure
Create a panel code for a particular drug. If the drug is billed at different amounts, a panel code may be set up for each billable amount. The panel code may be a single procedure panel or part of another panel containing multiple procedures. Complete the screen as normal with these fields included:
1.1 <Status> 
Set this field to 'N.' It is used to include the necessary NDC information when billing.
1.2 <Qty Calculation> 
This field determines whether or not the cursor stops at the <QTY> field on the Charges --►Charge screen when posting charges. Select the default, 'N', if the cursor does not need to stop at <QTY>.
• Set to 'Y' if quantities need to be adjusted during charge posting without affecting the charged amount.
• Set to 'X' if the quantity needs to be adjusted during charge posting and multiply the charged amount.
• This field works in conjunction with Utility --►Procedure --►Procedure <Global Y/N>. Refer to the online documentation for Utility --►Procedure --►Procedure before making any changes.
1.3 <NDC Number> 
Enter the 11-digit NDC code. Do NOT enter hyphens or the NDC Qualifier (the qualifier is added by Intellect). The National Drug Code number and Qualifier are submitted in the electronic claim Loop 2410, Segment LIN, or it prints on paper billing as shown in the example below.
1.4 <Unit of Measure> 
The Unit of Measure is required when an NDC Code is present. Select the Composite Unit of Measure Qualifier that applies to the billing:

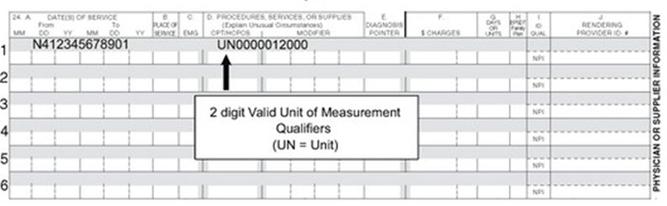
The Unit of Measure is used to populate the electronic 837 claim Loop 2410, Segment CTP05, or it prints on paper billing as shown in this example.
1.5 <NDC Unit Value> 
The NDC Unit Value indicates the billable portion of the total purchased unit.
Example 1: If the total amount in the purchased unit is 100 ml, and the billable amount is 50 ml, then the NDC Unit Value is .5 (50/100 = .5).
Example 2: If the total amount in the purchased unit is 50 mg, and the billable amount is 150 mg, then the NDC Unit Value is 3 (150/50 = 3).
Sample 837 EB file showing the NDC:
LIN**N4*NDC12345678 This is the NDC number
CTP****0.5*ML This is the NDC Unit Value from Utility --►Procedure --►Procedure
If the medication is in HCPCS units:
Before converting HCPCS/CPT units to NDC units, this information is needed:
• Amount of drug to be billed
• HCPCS/CPT code
• HCPCS/CPT code description
• Number of HCPCS/CPT units
• NDC (11-digit billing format)
• NDC description
• NDC unit of measure
Consider the following example for Ciprofloxacin IV 1200 MG (1 day supply):
| Amount of drug to be billed | 1200 MG |
| HCPCS/CPT code | J0744 |
| HCPCS/CPT code description | Ciprofloxacin for intravenous infusion, 200 MG |
| Number of HCPCS/CPT units | 6 |
| NDC (11-digit billing format) | 00409-4765-86 |
| NDC description | Ciprofloxacin IV SOLN 200 MG/20 ML |
| NDC unit of measure | ML |
How do I calculate the NDC units?
Here is a sample calculation based on the information on the table above for Ciprofloxacin IV 1200 MG (1 day supply).
• The amount of the drug to be billed is 1200 MG, which is equal to 6 HCPCS/CPT units.
• The NDC unit of measure for a liquid, solution, or suspension is ML; therefore, the amount billed must be converted from MG to ML.
• According to the NDC description for NDC 00409-4765-86, there are 200 MG of ciprofloxacin in 20 ML of solution (200 MG/20 ML).
• Take the amount to be billed (1200 MG) divided by the number of MG in the NDC description (200 MG). 1200 ÷ 200 = 6
• Multiply the result (6) by the number of ML in the NDC description (20 ML) to arrive at the correct number of NDC units to be billed on the claim (120). 6 x 20 ML = 120
When required by your practice, create a record on the appropriate encounter screen for each patient with a claim, based on the type of billing.
2.1 <Rx Number > 
Complete this field using the unique identification number assigned by the pharmacy or supplier for the prescription. The Rx Number is submitted in the electronic Loop 2410, Segment REF02, with Qualifier XZ automatically added by Intellect.
3.1 Post charges as usual.
3.2 <EN#> 
Complete this field with the encounter number containing the RX number for this patient.
3.3 <QTY> 
Modify the amount in the field, if necessary.
1. Professional Billing CMS 15000 (HCFA)
Box 24A (in the gray-shaded area) prints the NDC number proceeded by the 'N4' qualifier.

Box 24D (in the gray-shaded area) prints the quantity proceeded by the Unit of Measure qualifier.
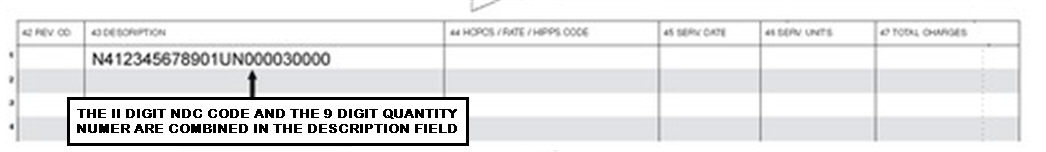
2. Institutional Billing UB04
Box 43, the Description field, prints the N4 Qualifier, NDC number, Unit of Measure and the Quantity.
3. Internal Control Number and Frequency Code on Paper Claim
You may now include the Internal Control Number and the Frequency Code on your paper claim if completed in the Charges --► Encounter <Claim Frequency Code> and <Internal Control Number> fields. Prior to this update, these claims were used only for electronic billing.
The Claim Frequency Code is used to advise the payor that the claim is either:
1 Original Submission (default used for electronic claims)
6 Corrected Claim
7 Replacement Claim
8 Void
The Internal Control Number is assigned by the payor and is usually found on the Explanation of Benefits.
NOTE: To utilize this feature, call PCS Support to have these fields added to the paper claim forms.