
Intellect™
3. CHARGES MENU OPTIONS
VII. Specialty Charges/NDC Set Up
Effective April 1, 2009, Medicaid and other insurance carriers began requiring NDC information for both paper and electronic billing. NDC information may be billed for both Professional and Institutional billing.
The Deficit Reduction Act (DRA) of 2005 required State Medicaid agencies to provide for the collection of NDCs on all claims for certain physician-administered drugs for the purpose of billing manufacturers for Medicaid drug rebates.
A physician-administered drug includes any covered outpatient drug provided or administered to a recipient, which is billed by a provider other than a pharmacy. Such providers would include, but not be limited to, physician offices, clinics, and hospitals. A covered outpatient drug is broadly defined as a drug that may be dispensed only upon prescription and is approved for safety and effectiveness as a prescription drug under the Federal Food, Drug and Cosmetic Act. Physician-administered drugs are not restricted to injectable drugs only. Physician-administered drugs include any drug regardless of the method of administration.
Such claims need to include NDCs, corresponding quantity amounts, Unit of Measure, and a prescription number for physician-administered drugs.
Follow this simple three-screen process when billing Medicaid for appropriate physician-administered drugs for electronic claims submission.
1. Create a Utility --►Procedure --►Procedure for the particular drug. This may be single panel or part of another panel. Complete this screen as normal with the following fields included:
1.1 <Status> ![]()
Set this field to "N". It is used to include the necessary NDC information when submitting the electronic claim.
[Name change effective version 13.10.29 - formerly QTY. (Y/N/X)]
This field determines whether or not the cursor stops at the QTY field when posting charges.
Set to "Y" if you will need to adjust quantities at posting.
1.3 <Cost> ![]()
Type the dollar amount of the cost. This field accepts decimal DD.CC, but no $.
1.4 <NDC Number> ![]()
This field is used for electronic billing of claims. If completed, the National Drug Code number is submitted in the electronic claim in Segment LIN, Loop 2410. Enter the 11-digit NDC code without hyphens or the qualifier (Intellect adds the qualifier).
1.5 <Unit of Measure> ![]()
The <Unit of Measure> is required when an NDC Code is present. Select the Composite Unit of Measure Qualifier that applies to the billing in this field. It is used to populate the Electronic 837 claim Loop 2410 CTP05.
F2 = International Unit
GR = Gram
ML = Milliliter
UN = Unit
1.6 <NDC Unit Value> ![]()
This field is used to convert quantities from HCPCS to NDC.
This value is used to populate the Electronic 837 claim Loop 2410 CTP04
Type the actual decimal quantity (or whole number) as computed, administered in a single dose relative to the purchase unit.
HCPCS Quantity (for a single panel) divided by NDC purchase unit = NDC Unit Value
For example:
HCPCS code is per 10mg and the product comes as a dry powder injection 500mg
NDC units are "each vial"
Dose was 100 mg, for example
HCPCS quantity = 10 and the NDC quantity = 100/500 = 0.2
Create a record on any of the encounter screens for each patient with a claim. Complete the <Rx Number >
![]()
Use the unique identification number assigned by the pharmacy or supplier for the prescription. This uses Loop 2410 REF02 with the Qualifier XZ automatically added by Intellect.
3. Charges --► Charge
Post charges as normal. Be sure to complete the <EN#> field with the encounter number containing the RX number for this patient.
![]()
Modify the amount in the <QTY>. This may be changed as necessary.
![]()
Paper Claims
Intellect completes Box 24A CMS 1500 (HCFA) in the gray shaded area with the NDC number proceeded by the "N4" qualifier.

- OR -
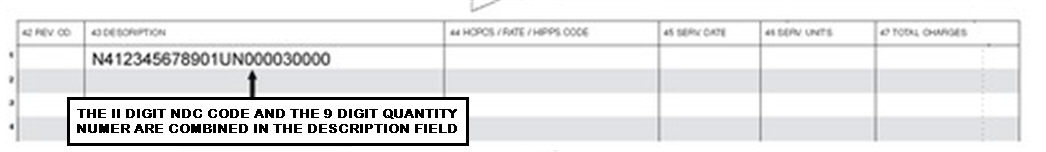
On the UB-04 claim form, Intellect completes the Description field (Box 43) including the Unit of Measure and the Quantity.
Intellect completes Box 24D CMS 1500 (HCFA) in the gray shaded area with the quantity proceeded by the Unit of Measure qualifier
