
Intellect™
CHARGES MENU OPTIONS

Specialty Charges
Medicare Billing Requirements for Anemia Therapies
CR 5699, from which this article is taken, instructs all providers and suppliers that:
1. Effective January 1, 2008, all claims billing for the administration of an ESA with HCPCS codes J0881, J0882, J0885, J0886 and Q4081 must report the most recent hematocrit or hemoglobin reading available when the billed ESA dose was administered. Facilities should bill at a frequency that allows for the reporting of the most recent hematocrit or hemoglobin reading prior to the start of the billing period that is applicable to the administrations billed on the claim. For new patients this would be the most recent reading prior to the onset of treatment. NOTE that a provider may have to submit more than one claim for the month if there were multiple readings that were applicable to the administrations given during the month. Claims submitted prior to the publication of change request 5699 that were not completed per the instructions in change request 5699 should be re-submitted.
For institutional claims, the hemoglobin reading is reported with a value code 48 and a hematocrit reading is reported with the value code 49. Such claims for ESAs not reporting a value code 48 or 49 will be returned to the provider.
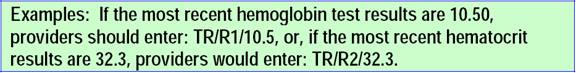
Effective for services on or after January 1, 2008, for professional paper claims, test results are reported in item 19 of the Form CMS-1500 claim form. For professional electronic claims (837P) billed to carriers or A/B MACs, providers report the hemoglobin or hematocrit readings in Loop 2400 MEA segment. The specifics are MEA01=TR (for test results), MEA02=R1 (for hemoglobin) or R2 (for hematocrit), and MEA03=the test results. The test results should be entered as follows: TR= test results, R1=hemoglobin or R2=hematocrit (a 2-byte alpha-numeric element), and the most recent numeric test result (a 3-byte numeric element [xx.x]). Results exceeding 3-byte numeric elements (10.50) are reported as 10.5.
Effective for dates of service on and after January 1, 2008, contractors will return to provider paper and electronic professional claims, or return as unprocessable paper and electronic institutional claims for ESAs when the most recent hemoglobin or hematocrit test results are not reported.
When Medicare returns a claim as unprocessable for ESAs with HCPCS codes J0881, J0882, J0885, J0886, or Q4081 for failure to report the most recent hemoglobin or hematocrit test results, it will include Claim Adjustment Reason Code 16 (Claim/service lacks information which is needed for adjudication.) and Remittance Advice Code MA130 (Your claim contains incomplete and/or invalid information, and no appeal rights are afforded because the claim is unprocessable. Please submit a new claim with complete/correct information.)
2. Effective January 1, 2008, all non-ESRD ESA claims billing HCPCS J0881 and J0885 must begin reporting one (and only one) of the following three modifiers on the same line as the ESA HCPCS:
• EA: ESA, anemia, chemo-induced;
• EB: ESA, anemia, radio-induced; or
• EC: ESA, anemia, non-chemo/radio
For CMS 1500 paper claims enter the test results in Charges --►Encounter --►Generic <Box 19 Claim notes>.
For Electronic Claims submission enter the test results in Charges --►Encounter --►Epogen <Measurement Value>.
• Non-ESRD ESA institutional claims that do not report one of the above three modifiers along with HCPCS J0881 or J0885 will be returned to the provider.
• Non-ESRD ESA professional claims that are billed without one of the three required modifiers as line items along with HCPCS J0881 or J0885 will be returned as unprocessable with reason code 4 and remark code MA130. If more than one modifier is reported, the claim will be returned with reason code 125 and remark code N63.
3. Effective January 1, 2008, all non-ESRD, non-ESA claims billing for the administration of Part B anti-anemia drugs used in the treatment of cancer that are not self-administered must report the most recent hematocrit or hemoglobin reading. Facilities should bill at a frequency that allows for the reporting of the most recent hematocrit or hemoglobin reading prior to the start of the billing period that is applicable to the administrations billed on the claim. For new patients this would be the most recent reading prior to the onset of treatment. NOTE that a provider may have to submit more than one claim for the month if there were multiple readings that were applicable to the administrations given during the month.
• Institutional claims that do not report the most recent hematocrit or hemoglobin reading will be returned to the provider.
• Professional claims that do not report the most recent hematocrit or hemoglobin reading will be returned as unprocessable
For CMS 1500 paper claims, enter the test results in Charges --► Encounter --► Generic <Box 19 Claim Notes> and attach that encounter when posting Charges --►Charge <EN#>.
For Electronic claims submission, enter the test results in Charges --► Encounter --► Epogen <Measurement Value> fields and attach that encounter when posting Charges --►Charge <EN#>.