
Intellect™
UTILITY MENU OPTIONS

Messages
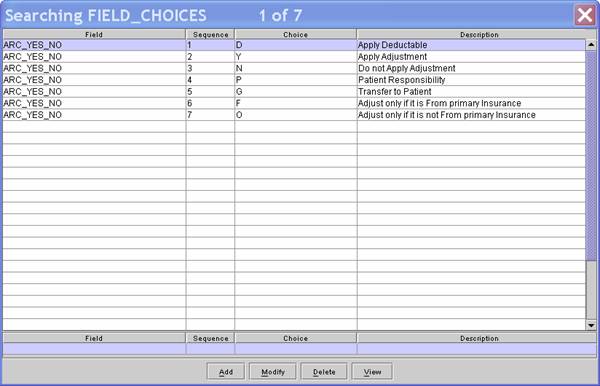
Reason Codes
Standard to Intellect are ERA Reason Codes which are accessed during Auto Posting. The coding determines which action should be applied and which should not. Previously, the conditions of when to apply segments and when to change the Who column were hard-coded within the program and could not be customized per clinic request. The system reads the reason codes embedded into the ERA file being posted and compares them to those set up in Utility --►Messages --►Reason Codes, and reads the 'Status' to determine whether to perform the action as defined. The code list is not automatically updated; clinics must manually make any additions or revisions.
It is very important not to delete existing reason codes or modify the code without instructions to do so from the Intellect staff.
1. To add a Reason Code in Intellect, go to Utility --► Messages --►Reason Codes --►Add
The Add REASON CODES screen opens:
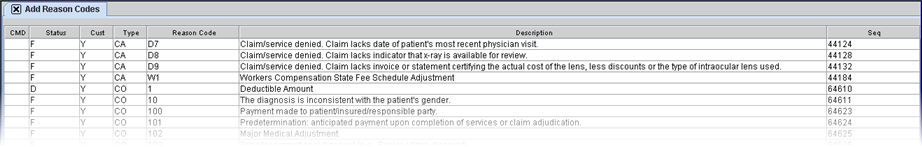
Effective 9.12.29, this screen was enabled with tooltip (hover on/over) capability. In other words, placing the mouse on a field causes the contents of that field to be displayed in a pop-up box. The columns were also re-sized in this version.
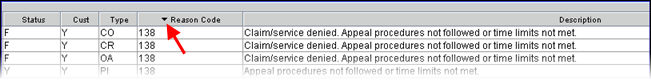
Note: To view the Reason Codes in order by the <Status>, <Customized>, <Reason Code>, or <Description> column, click once on the heading of the column. The system displays a down arrow to the right of the heading indicating the data is listed in descending order by that column:
2. CMD 
2.1 Enter 'A' (add), 'M' (modify), 'D' (delete), OR press [Esc] to clear.
2.2 This list of Reason Codes is generally maintained by the vendor and deletions are strongly discouraged as are modifying anything but the Status column.
NOTE: The 'Who' column reference in this document applies to Payment --► Open Item <W>, Ledger --► Open Item <Who>, and Ledger --► Accounting <Who>.
3.1 Options available in the Status column are:
3.1.1 Y: Yes – apply the adjustment regardless of whether or not a payment was made:
When posting for the Primary Insurance and the patient has a Secondary Insurance, the Who column changes to S
- OR -
When posting for the Secondary Insurance or the patient does not have Secondary Insurance, the Who column changes to G.
3.1.2 N: No – do NOT apply the adjustment. The Who column is NOT affected or changed.
3.1.3 D: Update the treatment history deductible. This option should be used only for ‘Deductible’ Reason Codes:
When posting for the Primary Insurance and the patient has a Secondary Insurance, the Who column changes to S
- OR -
When you are posting for the Secondary Insurance or the patient does not have Secondary Insurance, the Who column changes to G.
3.1.4 P: The Co-Insurance prints on the Automatic Payment Journal (Payment --► Auto Payment <Post Payment Report>). This option does not have any other affect and should be used only for ‘Co-Insurance’ Reason Codes.
3.1.5 G: No - do NOT apply the adjustment.
When posting for the Primary Insurance and the patient has Secondary Insurance, the Who column changes to S.
- OR -
When posting for the Secondary Insurance or the patient does not have Secondary Insurance, the Who column changes to G.
3.2 To view the list of codes with descriptions, press the [F2] key to display the Searching screen. To select the code from the list, either highlight the record and press the [Enter] key, OR double-click on the record.
4. Customized 
4.1 This field is used to protect the current entry from being overwritten.
4.2 Type 'Y' to protect OR 'N' to allow it to be overwritten.
5. Type 
5.1 The ‘Adjustment Group Type’ (Non-Medical Group Codes) identify either the financially responsible party or the general category of payment adjustment. A group code is always paired with a CARC (claim adjustment reason Code). Use these codes to define which ERA adjustments to apply and which not to apply based on a combination of the <Type> and <Reason Code>. Previously, only the <Reason Code> was used to determine whether or not to apply an adjustment. For example: If an office does not accept assignment from a payor, the office may choose to apply Reason Code 42 - Charges exceed our Fee Schedule or Maximum allowable Amount for some Adjustment Group Type codes, yet not apply the adjustment to other codes.
5.2 Available Types:
|
Code |
Description |
|
CA |
Manual Claim Adjustment |
|
CO |
Contractual Obligation - Used when a contractual agreement between Medicare and the provider, or a regulatory requirement, resulted in an adjustment. When 'CO' is used to describe an adjustment, a provider is not permitted to bill the beneficiary for the amount of that adjustment. |
|
CR |
Correction and Reversal - Used for correcting a prior claim. It applies when there is a change to a previous adjudicated claim. |
|
OA |
Other Adjustment - Used when no other Group Code applies to the adjustment (NOTE: ALL ODJFS error codes are mapped to this type). |
|
PI |
Payor Initiated Reductions - Used when, in the opinion of the payer, the adjustment is not the responsibility of the beneficiary. NOT USED BY MEDICARE. |
|
PR |
Patient Responsibility - Represents an adjustment amount that is billed to the beneficiary or insured. This Group Code is typically used for deductible and coinsurance adjustments. |
6. Reason Code 
6.1 Effective version 9.12.29, Electronic Remittance Advice/Notice (ERA/ERN) Reason Codes for Payor Initiated Reductions (Type: PI) have been added to the Utility --►Messages --►Reason Codes table. PI Reason Codes are used when, in the opinion of the payer, the adjustment is not the responsibility of the beneficiary. The PI Reason Codes are NOT used by Medicare.
6.2 ERA Reason Codes are accessed during Auto Posting. The coding determines which action should be applied and which should not. The system reads the reason codes embedded into the ERA file being posted, compares them to those set up in the <Reason Code> column, and reads the <Status> to determine whether to perform the action as defined. Offices should review the new PI Reason Codes and determine how they want the adjustments handled when posting the ERA/ERN via Auto Posting. Intellect ALWAYS posts the payment. An office may decide whether or not to apply the Adjustment, and whether or not the Who column should change. See <Status> for available options.
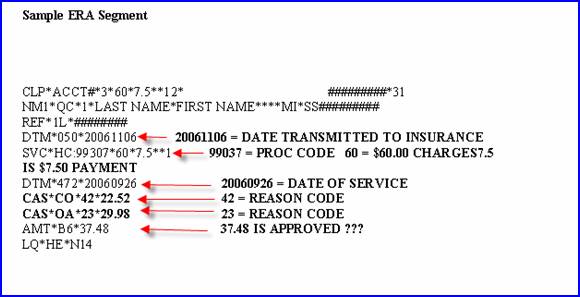
NOTE: The ERA file may include multiple segments for a single service/charge. Each segment is handled separately, based on the option (Status) selected for the Reason Code. The Automatic Payment Journal prints up to four Reason Codes. To see any additional Reason Codes, print the EOB from Easy Print.
7. Description 
7.1 The description of the code may be modified if desired.
8. Sequence 
8.1 This number is generated by the system’s underlying database.