

OnSTAFF 2000
CMS 1500 CLAIM FORM REVIEW
Please use this as a guide in assisting you with completing your billing forms accurately. Each box of the CMS 1500 claim form is reviewed. Noted per box is the exact System location of the printed information and billing method criteria when applicable.
Read July 25, 2008 Palmetto Instructions
Box 1 MEDICARE, MEDICAID, CHAMPUS, CHAMPVA, GROUP HEALTH PLAN,FECA BLK LUNG, OTHER
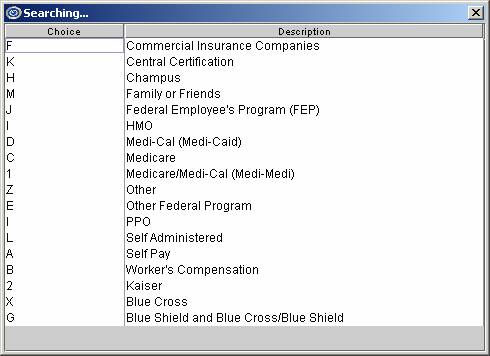
The appropriate box will be checked according to the type of insurance entered in the Utility --►Insurance <Insurance Type> field. With the cursor on this field, pressing [F2] will display the following list:
*837 Electronic Claims Submission Equivalent Loop 2000B SBR09
This will print the insurance I.D. from the Registration --►Patient --► Insurance screen <Subscriber No.> field.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM109
Box 2 PATIENT’S NAME
This will print the patient name from the Registration --►Patient <Last Name>, <First Name>, <Middle Initial> fields.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 103,04,05,07
This will print the birth date of the patient from the Registration --►Patient <DOB> field.
*837 Electronic Claims Submission Equivalent Loop 2010BA DMG02
If the patient is a dependent OR you are printing a secondary claim form AND other than self is the insured, then the name of the insured will print from the Registration --► Patient --►Insurance screen <Last Name>, <Insured First Name>, <Middle Initial> fields.
If the patient is the insured when billing Medicare as their secondary coverage, then “SAME” will print here.
For Workers Compensation Patients (Utility --►Category Type (C/P/W/O/F/G) = W) Registration --► Worker --► Insurance <Employer> will be used.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 103,04,05,07
Box 5 PATIENT’S ADDRESS, CITY, STATE, ZIP CODE, TELEPHONE
The full address and phone number of the patient will print from the Registration Patient <Address>, <Zip Code>, <City>, <State>, and <Home Phone No> fields.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 301,02
The appropriate box will be checked based on the information entered on the Registration --► Patient --► Insurance screen <Relationship to Insured> field. Valid field entries are:
18 - Self
1 - Spouse
19 - Child
- Other
*837 Electronic Claims Submission Equivalent Loop 200B SBR02 PAT01
B insured will print from the Registration --►Patient --► Insurance <Address>, <Zip Code>, <City>, <State>, and <Home Phone No> fields.
If the patient is the insured when billing Medicare as their secondary coverage, then ““SAME”” will print here.
For Workers Compensation Patients (Utility --►Category Type (C/P/W/O/F/G) = W) Registration --► Worker --► Insurance <Address>, <Zip Code>, <City>, <State>, and <Phone> fields. will be used.
*837 Electronic Claims Submission Equivalent Loop 2010BA N301,02
MARITAL:
This will mark the appropriate marital status box according to the entry in the Registration --► Patient (or Worker ) <Marital Status (S/M/D)>. Valid selections are:
S: the “Single” box will be marked
M: the “Married” box will be marked
D: the “Other” box will be marked
EMPLOYED:
The employed box will be marked according to the selection in the Charges --► Encounter <Status: Employment> field when that encounter is associated with the charges being printed Charges --►Charge OR Charges --► Modify <EN#> field.
FULL-TIME/PART-TIME STUDENT:
This will mark the student status boxes according to the entry in the Charges --► Encounter <Status Student (F/P/N)> field from the patients Encounter screen when that encounter is associated with the charges being printed Charges --► Charge OR Charges --►Modify <EN#> field. Valid selections are:
F: the “Full-Time Student” box will be marked.
P: the “Part-Time Student” box will be marked.
If there is not an entry in this field, then the boxes will be left blank.
When billing the primary, if the patient is the insured for the secondary coverage,” “SAME”” will print here.
If the patient is a dependent, System will print the Insured’s name from <Last Name>, <Insured First Name>, <Middle Initial> fields from the Registration --► Patient secondary Insurance screen.
*837 Electronic Claims Submission Equivalent Loop 2330A NM 103,04,05,07
.
If the patient is a Medi-Medi patient (Medicare primary and Medi-Cal (Medicaid) secondary) System will print the ID obtained from the Registration --► Patient <Subscriber No.> field of the patients Medi-Medi insurance coverage screen.
All other cases with secondary coverage, prints “MG” for Medigap plans plus the value found in the Registration --► Patient secondary insurance screen <Subscriber No.> field.
*837 Electronic Claims Submission Equivalent Loop 2320 SBR03 /2330A REF02
If the patient is the insured, the date of birth and sex will print from the Registration --► Patient --► <DOB> and <Gender> fields.
If the patient is a dependent, the date of birth and sex of the insured will print from the Registration --► Patient --►Insurance <Insured DOB> and <Gender> fields.
*837 Electronic Claims Submission Equivalent Loop 2320 DMB02 and 2320 DMG03
If the patient is a dependent on the secondary coverage, the name of the employer will print from the Registration --►Patient secondary Insurance screen <Insured Employer> field.
If the insurance coverage is secondary to Medicare, the name of the secondary insurance will print here from the Utility --►Insurance <Name>.
Use Utility --►Insurance <OCNA> 5 digit COBA ID for automatic crossover.
*837 Electronic Claims Submission Equivalent Loop 2320 SBR04/2320 NM103
a: EMPLOYMENT (CURRENT OR PREVIOUS)
The YES or NO box will be marked according to the entry in the Charges --► Encounter <Employment (Y/N)> when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
This will mark the YES box only if an A is entered in the Charges --► Encounter <Related: Accident > field. Will enter the patient’s state of residence.
If this field is blank or contains a value other than A, the NO box will be marked.
c: OTHER ACCIDENT
This will mark the YES box only if an O (alpha O) is entered in the Charges --► Encounter <Related: Accident > field when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field). If this field is blank or contains a value other than O, the NO box will be marked.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM11 EM, CLM11 AA, CLM11 OA, CLM11, CLM11 AP
Should print MCD for Medigap crossovers.
If Medi-Cal is primary (Utility --► Insurance <Insurance Type> =D, and Charges --► Encounter --► Generic <Share of Cost Amount> has an entry it will print here.
If the Medicare or Medi-Cal (Medicaid) is primary (Utility --► Insurance <Insurance Type> = C or D), the word “NONE” will print here.
If there is Insurance primary to Medicare, Registration --► Patient --► Insurance screen <Group No.> field will print here.
If the patient has a workers comp category type (Utility --► Category <Type (C/P/W/O/F/G)> = W or F) the field will be left blank.
All other cases with secondary coverage the value entered on the patient’s Registration Patient insurance screen <Group No.> field will print here.
Note:
For a CMS-1500 paper claim to be considered for Medicare Secondary Payer benefits, a copy of the primary payer's explanation of benefits (EOB) notice must be forwarded along with the claim form.
*837 Electronic Claims Submission Equivalent Loop 2000B SBR 03
If Registration --► Patient --► Insurance <Relation to Insured> not = 18
the patient’s date of birth and sex from the patient’s Registration --► Patient <DOB> and <Sex (M/F/U)> fields will print here.
*837 Electronic Claims Submission Equivalent Loop 2010BA DMG02 and DMG03
When billing secondary, if Medicare is entered as the secondary coverage or if there is Medigap coverage in addition to Medi-Medi coverage, the entry from the patient’s Registration --►Patient <Employer Name> field will print here.
All other cases when billing secondary, System will print the entry from the patient’s Registration --► Patient secondary Insurance screen <Insured Employer> field.
All cases with secondary coverage will print the Registration --► Patient
--► Insurance screen <Claim No.> field entry when it’s Utility --►Insurance <Type> does not equal C.
*837 Electronic Claims Submission Equivalent Loop 2000B SBR 04
For all insurance with secondary the YES box will be marked.
MEDICARE DOES NOT REQUIRE AN ENTRY
SIGNED: The patient’s Utility --►Insurance <HCFA Box 12 & 13> field entry will print here.
DATE : Utility --►Set Up --►Clinic <Current Entry Date> will print here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM09 O106
Box 13 INSURED’S OR AUTHORIZED PERSON’S SIGNATURE
The patient’s Utility --►Insurance <HCFA Box 12 & 13> field entry will print here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM08 2320 O103 CLM10 2320 O104
If the patient has a Worker’s Comp category (Utility --►Category <Type (C/P/W/O/F/G)> = W or F), this information prints from Charges --►Worker Encounter <Injury Date> field when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
For all other category types, this information prints from the patient’s screen Charges --► Encounter <First Symptom> field when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This information prints from the patient’s Charges --►Encounter Generic <First Consulted> field when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This information prints from the patient’s Charges --► Encounter <Unable To Work From> and < Unable To Work To> fields when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --► Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
For All Options below: If the referral source entered is not a physician (Utility --►Referring <Doctor/Other (D/O)> = O), System will print the treating physicians name from the Utility --►Provider <Name> field when the Utility --► Insurance Type is not D, F or 5 (in which case will be blank).
The name of the referral source (Utility --►Referring <Name> entry) will print here dependent on the field entry at Utility --►Set Up --►Parameter <Referring (P/C/F)>. Valid choices and where the printed information pulls from are:
P: Use referral from patient file
C: Use the referral entered at the time of posting charges (Charges -- ► Charge <Ref Prv>.
F: Look first to the referral entered at the time of posting charges (Charges -- ► Charge <Ref Prv>. If no referring doctor was entered at the time of posting charges: look to the patient file.
*837 Electronic Claims Submission Equivalent Loop 2310A NM 103,04,05,07
Following the above criteria for box 17:
17a Will print the associated identification number as requested in Utility --► Insurance <Box 17a> from either Utility --►Referring or Utility --►Provider
For proper billing the selection in Utility --► Insurance <Box 17a> should match Utility --► Insurance <Referring Type > which will provide the qualifier for 17a
Following the above criteria for box 17:
17b will print either Utility --►Referring <NPI> or Utility --►Provider <NPI>.
*837 Electronic Claims Submission Equivalent Loop 2310A NM109
This will print the Charges --► Encounter <Hospitalization From> and <Hospitalization To> when that encounter number is associated with the charges being printed (Charges --►Charge OR Charges --► Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This will print from the Charges --► Encounter <Box 19 Description> appended by <HCFA Box 19 Date > when the encounter number is associated with the charges being printed (Charges --►Charge OR Charges --► Modify <EN#> field).
For Anesthesiology billing when Utility --►Insurance Type = D (Medi-Cal/Medicaid) System will print "Start Time", "End Time", and "Total Time" in military units..
If Utility --►Procedure <Status> = “L” lab
And if Charges --► Encounter <Outside Lab> is configured with a facility code then Intellect will place an “X” in the Yes box of Outside Lab and under the $CHARGES heading, will print the total cost for all charges where the Utility --►Procedure <Cost> field has an entry.
If posting charges without Charges --► Encounter <Outside Lab> then under the $CHARGES heading, will print ‘NO PURCH SVC’.
*837 Electronic Claims Submission Equivalent Loop 2300 AMT02
Note: When the “yes” box form Item 20 (Outside Lab") is checked, Item 32 of the
claim form must be completed. When billing for purchased diagnostic tests the provider of service must identify the supplier’s name, address, zip code, and NPI in Item 32 of the claim form.
This will print in 21-1 through 21-4, based on the order entered at the time of posting (Charges --►Charge <Code>) , the ICD-9 codes from the Utility --►Diagnosis <ICD9 Code> field for the dates of service(s) requested.
*837 Electronic Claims Submission Equivalent Loop 2300 HI01, HI02, HI03, HI04
This will print the Charges --► Encounter <Medicare Status> code when the encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
Original Reference No
*837 Electronic Claims Submission Equivalent Loop 2300 REF02
If the patient has Medi-Cal (Medicaid) insurance coverage (Utility --►Insurance <Insurance Type> = D) this will print the Charges --►Encounter <Authorization No.> entry when the encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
Utility --► Provider <CLIA> Number if the following conditions are met:
Utility --► Insurance <CLIA > = “Y’ for insurance being billed
and Utility --► Procedure <Status> = “L” for the billed procedure.
If charges are linked to an encounter, the CLIA field entry from Charges Encounter <Authorization No> will override entry made on this screen.
*837 Electronic Claims Submission Equivalent Loop 2300 REF02/2300REF02 (REF01=X4,G1,9F)
FROM: When entering charges (Charges --►Charge <From/Date>) entry will print as the FROM date.
TO : For all procedures whose Utility --►Procedure <Global (Y/N)> = N, when entering charges (Charges --► Charge <To>) System will enter a TO date that is equal to the FROM date.
For all procedures whose Utility --►Procedure <Global (Y/N)> = Y, when entering charges (Charges --►Charge <To>) will be entered as the "TO' date (creating a range).
*837 Electronic Claims Submission Equivalent Loop 2400 DTP03
Based on the posted Charges --►Charge <Facility> code System reads Utility --► Facility. The Utility --►Facility <Place Of Service> code will print here.
*837 Electronic Claims Submission Equivalent Loop 2400 SV105
If the patient’s insurance coverage is Medi-Cal (Medicaid) (Utility --► Insurance <Insurance Type> = D) this will print from the patient’s Encounter screen <Emergency (Y/N)> field (Charges/Encounter) when the encounter number is associated with the charges being printed (Charges --►Charge OR Charges --► Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2400 SV109
Based on the patient’s assigned insurance Utility --►Insurance <Code (R/C/E/U)> field entry, the corresponding code from Utility --►Procedure < Code R>, <Code C>, <Code E>, <Revenue Code>and <Modifier R>, <Modifier C>, <Modifier E> (or modifier entered at the time of posting (Charges --►Charge <Code>) will print here.
*837 Electronic Claims Submission Equivalent Loop 2400 SV101
This will print the <RDX> field entry for charges being printed (Charges --► Charge OR Charges --►Modify).Medicare will only accept one related diagnosis per charge/procedure.
*837 Electronic Claims Submission Equivalent Loop 2400 SV107
This will print the amount from the posted Charges --► Charge <Charge>.
This amount is derived from Utility --►Procedure <Charge> field if a fee schedule has not been set up for the provider, insurance company and panel code being requested (Utility --►Procedure --►Fee Schedule).
If a Utility --►Procedure --►Fee Schedule is set up for the provider, insurance company and panel code requested and the <Alt. Charge> amount will be used.
*837 Electronic Claims Submission Equivalent Loop 2400 SV102
The value entered in the Utility --►Procedure <Days & Units> field will print here. If this value is modified at the time of posting, then the Charges --►Charge <Qty> entry will print.
*837 Electronic Claims Submission Equivalent Loop 2400 SV104
If the patient’s insurance coverage is Medi-Cal (Medicaid) Utility --►Insurance <Insurance Type> = D this will print the selected code number from the patient’s Charges --►Encounter --► Generic <Family Planning> field when the encounter number is associated with the charges being printed (Charges --►Charge OR Charges --►Modify <EN#> field).
*837 Electronic Claims Submission Equivalent Loop 2400 SV111
Uses the selection from Utility --► Insurance < Type> to print the rendering provider’s legacy number qualifier for the Id as requested by this insurer.
*837 Electronic Claims Submission Equivalent Loop 2010AA REF01
Regardless of billing method, will select and bill based on the program’s hierarchy.
System will first look in the Utility --►Provider --►Provider Facility screen
for a match of the Billing Provider, Insurance, and Facility. If a match is not found the program will look to Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance. If a match is not found in either table: System will use the information set up in the Utility --► Provider screen.
Then dependent upon Insurance <Selection (1/2/3)> for insurance being billed
FOR:
LEGACY NUMBERS
Provider Facility: System will complete the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry <HCFA Box 24 J>.
Provider Provider: System will complete the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry<HCFA Box 24 J>.
Provider: System will complete the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry in <HCFA Box 24 J1>, <HCFA Box 24 J2>, or <HCFA Box 24 J3>.
*837 Electronic Claims Submission Equivalent Loop 2310B REF02
NPI NUMBERS
Provider: System will complete the lower portion (NPI) of Box 24 J with the entry from Utility --►Provider --►< NPI >
*837 Electronic Claims Submission Equivalent Loop 2310B NM109
If your billing method is clinic (Utility --►Set Up --►System <Billing> = C OR "Blank" with Utility --►Category <Billing (D/C/N)> = C) the Utility --►Set Up --► Clinic <IRS ID NO.> will print here and the EIN box will be marked.
If your billing method is doctor (Utility --►Set Up<Billing> = D OR "Blank" with Utility --►Category <Billing (D/C/N)> = D)
OR
The Provider <Social Security No.> field will print marking the SSN box.
When both <I.R.S. Id> AND <Social Security No.> fields have entries, the <I.R.S. Id> will print here and the EIN box will be marked.
*837 Electronic Claims Submission Equivalent Loop 2010AA/AB NM109, NM 108
Box 26 PATIENT’S ACCOUNT NO
This box will print the patient’s account number from Registration --► Patient <Patient’s Account No.> field.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM01
If Y has been entered in the Registration -►Patient-► Insurance<Assignment> field, then the Yes box will be marked. If N has been entered, then the No box will be marked.
If the patient's insurance screen <Assignment> field default was modified at the time of posting charges or through the Charge --►Modify screen, then the Charges --► Charge OR Charges --►Modify <ASI> field entry will print here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM07
Box 28 TOTAL CHARGE
The sum of all the charges, boxes 24/1 through 24/6 on the claim form, will print here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM02
This box will print based on the entry at Utility --►Insurance <Include Payment>. Valid entries are:
Y Prints the total payment posted to the charges in box 24/1 through
24/6 and the sum of charges minus payments in Box 30
A Total payment plus adjustment posted to the charges in box 24/1 through 24/6 and the sum of charges minus payments and adjustments in Box 30.
N Prints 0.00. in Box 29 and total charges in Box 30
*837 Electronic Claims Submission Equivalent Loop 2300 AMT02
The current entry date will print here from Utility --►Set Up --►Clinic <Current Entry Date>.
If Utility --► Insurance <Provider Name (Y/N/X/Z)> = X or Z, the Utility --► Provider <Name> will print here.
*837 Electronic Claims Submission Equivalent Loop 2010AA, 2010 /B AIR 2310 NM1
N3, N4 REF Loop 2010AA, AB,PRV103 BHT03
System will print the Utility --►Facility <Name>, <Address>, <City>, <State>, and <Zip Code> field entries for the code entered when posting Charges --► Charge <Facility> OR Charges --►Modify <Facility>
Note: When the “yes” box form Item 20 (Outside Lab") is checked, Item 32 of the
claim form must be completed. When billing for purchased diagnostic tests the provider of service must identify the supplier’s name, address, zip code, and NPI in Item 32 of the claim form.
*837 Electronic Claims Submission Equivalent Loop 2310 C/D NM101
2310D NM103 OR 2310C NM109 (TIN) N3 & N4
System will print the Utility --►Facility <NPI>
*837 Electronic Claims Submission Equivalent Loop 2310D NM109
According to the patient's Utility --► Insurance <Selection 1, 2, 3> field entry, one of the following Utility --►Facility :< Provider 1>, :< Provider 2>, or
<Provider 3>.
If the charges are related to Mammography Utility --► Procedure <Mammography> will print here when the Procedure <Status> = “M” is posted.
*837 Electronic Claims Submission Equivalent Loop 2310D REF01 REF02
If your billing method is clinic (Utility --► Set Up --► Parameter <Billing Method> = C OR L with Utility --►Category <Billing (D/C/N)> = C) the following will print.
From Utility --►Set Up --►Clinic <Name>, <Address>, <City>, <State>, and <Zip Code> fields.
If your billing method is doctor (Utility --► Set Up --► Parameter <Billing Method> = D OR L with Utility --►Category <Billing (D/C/N)> = D) the following will print:
PHYSICIAN’S NAME, ADDRESS, CITY, ZIP CODE & PHONE
From Utility --►Provider <Organization Name>, address, city, state and zip code fields. If <Organization Name> field is blank, then this will print the <Name>, address, city, state and zip codes fields. When both the <Organization Name> and <Name> fields are filled in, the <Organization Name> field will print along with the address, city, state and zip code fields.
*837 Electronic Claims Submission Equivalent Loop 2010 AA OR 2010 AB NM1, N3, N4 PER
If your billing method is clinic (Utility --► Set Up --► Parameter <Billing Method> = C OR L with Utility --►Category <Billing (D/C/N)> = C) the following will print:
Utility --► Insurance <Group NPI>
If your billing method is doctor (Utility --► Set Up --► Parameter <Billing Method> = D OR L with Utility --►Category <Billing (D/C/N)> = D)
System will first look in the Utility --►Provider --►Provider Facility screen
for a match of the Billing Provider, Insurance, and Facility. If a match is not found the program will look to Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance. If a match is not found in either table: System will use the information set up in the Utility --► Provider screen.
Based on this hierarchy one of the following will print:
Provider Facility: <Group NPI>.
Provider/ Provider: <Group NPI>.
Provider: <Group NPI>.
*837 Electronic Claims Submission Equivalent Loop 2010AA NM109
After Dual use period for NPI expires this field will be only for Atypical Providers.
If your billing method is clinic (Utility --► Set Up --► Parameter <Billing> = C OR L with Utility --►Category <Billing (D/C/N)> = C) the following will print:
Utility --► Insurance <Insurance Type> (The qualifier) followed by
Utility --► Insurance <1500 Form Box 33 Group>.
If your billing method is doctor (Utility --► Set Up --► Parameter <Billing > = D OR L with Utility --►Category <Billing (D/C/N)> = D)
System will first look in the Utility --►Provider --►Provider Facility screen
for a match of the Billing Provider, Insurance, and Facility. If a match is not found the program will look to Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance.
Based on this hierarchy one of the following will print:
Provider Facility: <HCFA Box33>.
Provider/Provider: <HCFA Box33>.
If a match is not found in either table: System will use the information set up in the Utility --► Provider screen.
Then dependent upon Insurance <Selection (1/2/3)> for insurance being billed
the following will print:
Utility --► Provider <HCFA BOX 33.1>
Utility --► Provider <HCFA BOX 33.2>
Utility --► Provider <HCFA BOX 33.3>