
OnSTAFF 2000
INSURANCE/PAY PLAN
PAY PLAN MENU
This option is used in adding and maintaining insurance contracts for conversion rate/unit value, fee schedule and capitated contract agreements.
Menu Options:
Pay Plan Used to define coverage information such as copayment and deductible amounts, days to bill, stop loss, authorization and eligibility phone numbers and more. This option also tells On-Staff if the contract is based on Conversion Rates and Unit Values or a Fee Schedule.
Diagnosis For use with capitated contracts. Used to carve out all charges related to a diagnosis, flagging that charge as fee for service.
Procedure For use with capitated contracts. Used to carve out charges that should be flagged as fee for service.
Insurance Used to set up a warning as well as list procedure codes that an insurance company does not pay on.
Insurance/Pay Plan/PAY PLAN
This option is used to set the coverage levels, co-payments and deductibles for insurance policies. For example, once this library is set up you can tell On-Staff that the patient has Pay Plan AETNA and all coverage information will be defined for that patient. When all pieces are in place (/Utility/Procedure <Conversion 0 (1, 2, 3, 4)> field completed, /Utility/Pay Plan/Pay Plan completed, /Utility/Procedure/Fee Schedule completed for Fee Schedule contracts, /Utility/Insurance/Pay Plan/Pay Plan <Plan Code> assigned to the patient’s primary insurance) On-Staff will display the patient's responsibility due after primary insurance payment when posting charges, thus allowing you to collect this portion from the patient at the time of the visit. On-Staff will display the contractual allowed amount when posting payments, thus allowing you to determine if payment is per contract amount or needing appeal for underpayment.
Menu Options:
Add Add a new Pay Plan
Modify Modify an existing Pay Plan
Delete Delete an existing Pay Plan
View View an existing Pay Plan
Print Prints a listing of the information in this file.
Exit Returns you to the Insurance Menu.
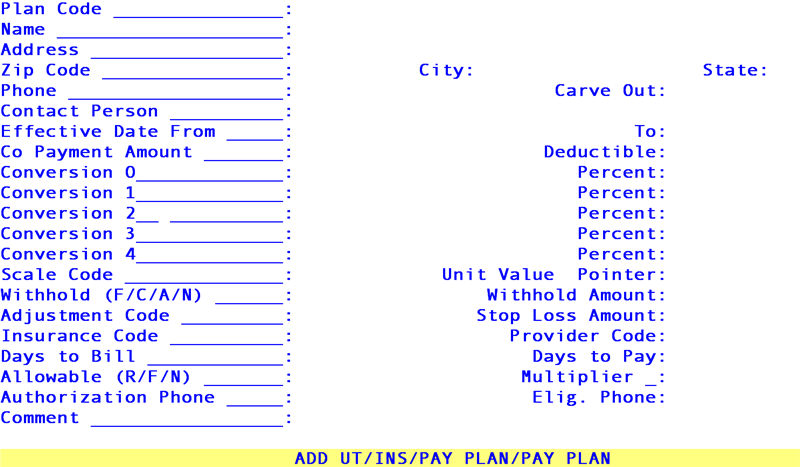
When the Add option is selected, On-Staff will display the following fields:
Plan Code: Enter the user assigned internal code for this pay plan, up to six characters of letters and/or numbers.
Name: Enter the user defined name for this pay plan, usually the name of the contracting IPA or HMO insurance company.
The Address through Phone fields are informational only and may be left blank.
Address: Enter the street address for this pay plan.
Zip code: Enter the zip code for this pay plan.
City: Enter the city for this pay plan.
State: Enter the state for this pay plan.
Phone: Enter the phone number for this pay plan.
The Carve Out field is completed ONLY when setting up pay plans for capitated contracts and otherwise will be set to N or left blank. This field allows you to override the /Utility/Procedure <HMO Adjust> field entry of N with the following contractual conditions. Items carved out will not be captured when posting your monthly cap check using the /Payment/Auto Payment feature (charges captured through this feature are determined by their /Procedure <HMO Adjust> field entry of N).
Carve Out: Press the [F2] search key to display the following valid choices:
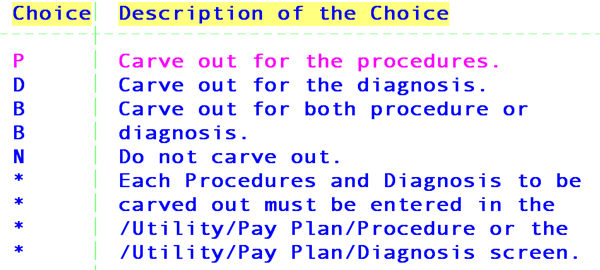
See CONTRACT EXAMPLES, Example 1,
The Contact Person through Deductible fields are informational only and may be left blank.
Contact Person: Enter the name of the contact person.
Effective
Date From: Enter the effective date of this pay plan’s contract.
This is an informational field that will automatically default into the New Patient Insurance screen Coverage From field when the Plan Code field entry for this pay plan is entered into the New Patient Insurance screen Pay Plan field.
The patient's effective date of coverage will likely be different. Simply override the default by entering the patient's effective date in the New Patient Insurance screen Coverage From field. This will override but not change the Effective Date From field entry here.
To: Enter the termination date of this pay plan’s contract.
This is an informational field that will automatically default into the New Patient Insurance screen coverage To field when the Plan Code field entry for this pay plan is entered into the New Patient Insurance screen Pay Plan field.
The patient's insurance coverage termination date will likely be different. Simply override the default by entering the patient’s termination date in the New Patient Insurance screen coverage To field. This will override but not change the To field entry here.
When the provider's contract terminates, run an aging report by insurance to obtain all patients with balances in order to update each patient's New Patient Insurance screen.
Co Payment
Amount: Enter the most common copayment amount for this pay plan or if desired, leave blank.
This is an informational field that will automatically default into the New Patient Insurance screen Co Payment field when the Plan Code field entry for this pay plan is entered on the New Patient Insurance screen Pay Plan field.
Copayment amounts vary. Simply override the default by entering the patient’s copayment in the New Patient Insurance screen Co Payment field. This will override but not change the Co Payment Amount field entry here.
Deductible: Enter the most common deductible amount for this pay plan.
This is an informational field which will automatically default into the New Patient Insurance screen Deductible Met field when the Plan Code field entry for this pay plan is entered in the New Patient Insurance screen Pay Plan field.
Deductible amounts vary. Simply override the default by entering the patient’s deductible in the New Patient Insurance screen Deductible Met field. This will override but not change the Deductible field entry here.
The Conversion 0 through Conversion 4 fields are completed ONLY when setting up pay plans with conversion rate/unit value based contractual agreements and otherwise will be left blank.
Conversion 0 through
Conversion 4: To allow for flexibility in setting up conversion rates, enter the contractual conversion rates in their respective fields. As a suggestion:
Conversion 0 may be used for surgery
Conversion 1 may be used for medical
Conversion 2 may be used for anesthesiology
Conversion 3 may be used for radiology
Conversion 4 may be used for pathology
The /Utility/Procedure < Conversion> field entry will specify which /Pay Plan <Conversion 0 (or 1, 2, 3, 4)> field to use when posting that procedure. See FIG. 1.
The following Percent fields are completed when setting up pay plans for conversion rate/unit value OR fee schedule contractual agreements.
Percent fields: Enter the contractual percent (e.g., 80 for 80 percent) which is the percentage of the approved amount the insurance will pay.
Each Percent field is associated with the Conversion 0 (or 1,2, 3, 4) field to the left of the Percent field. The /Utility/Procedure <Conversion> field entry will specify which Percent field to use when posting the procedure. See FIG. 1.
See CONTRACT EXAMPLES, Example 2,
FIG. 1:
/Utility/Procedure:
Days & Units : Assignment(Y/N) : Conversion : 1 ç
/Utility/Insurance/Pay Plan/Pay Plan:
Conversion 0 : 7.15 Percent: 100.00
Conversion 1 : 5.75 Percent: 80.00
Conversion 2 : 6.75 Percent: 80.00
Conversion 3 : 3.15 Percent: 80.00
Conversion 4 : 5.15 Percent: 100.00
é*
é* This column is generally completed only when setting up a pay plan based on a conversion rate/unit value contract, although, a combination of conversion rate/unit value AND fee schedule fields is possible. Contact your Trainer or a Software Support Representative with questions.
The Scale Code field is completed ONLY when setting up a pay plan for a conversion rate/unit value based contractual agreement and otherwise will be left blank. This field allows for different unit value scaling systems between contracts.
Scale Code: Enter the user defined code for the scaling system (i.e., set of unit values) used by this insurance contract.
This field is used to determine which scaling system (/Utility/Procedure/Unit Value <Scale Code>) to use to get the unit values. If this field is blank, the /Utility/Procedure < Unit Value> field entry will be used. The following are a few known scales, others may apply to your practice:
McGraw Hill
RBRVS
CRVS
The Unit Value Pointer field MUST BE ENTERED when the Scale Code field is entered.
Pointer: Enter which unit value (1, 2, 3) is to be used.
This field is used to determine which unit value in the scaling system (indicated in the above entered Scale Code field) to use. The /Utility/Procedure/Modifier < Charge (G/P/T)> field entry will specify which column to use, Global or Prof.. The difference between the Global and Prof. column entries will be the technical unit value. See FIG. 2.
Press the [F2] search key to display the following valid choices:
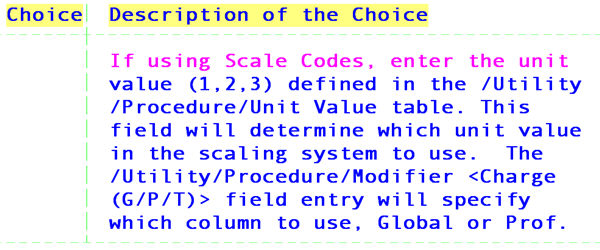
See CONTRACT EXAMPLES, Example 3
The Withhold (F/C/A/N), Withhold Amount, and Adjustment Code fields are completed ONLY when setting up a pay plan whose contractual agreement includes withhold amounts, otherwise these fields will be blank (or zero).
These fields are used to accommodate insurance contracts that allow for an additional administrative adjustment of a charge which they call a ‘withhold’. This adjustment is not to be confused with the contracted provider adjustments calculated from the approved amounts (i.e., PPO adjustments). Certain procedure codes may not be subject to a withhold adjustment. These are flagged by setting the /Utility/Procedure <Withhold> field entry to N. For more information see Session II’s /Utility/Procedure section regarding the field <Withhold (Y/N)> and/or ask your trainer for the Software Requirements For Withhold Posting handout.
Withhold
(F/C/A/N): This field together with the Withhold Amount field is used to determine the actual amount to be withheld. Press the [F2] search key to display the following valid choices:
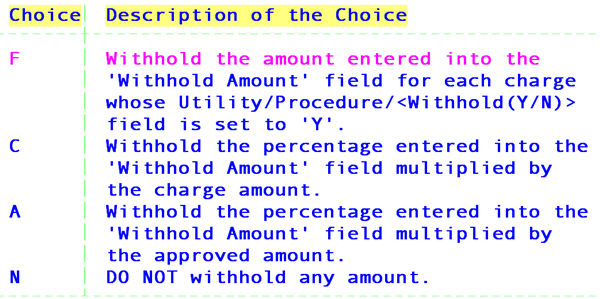
NOTE: You may choose to adjust or not adjust the withhold amount at the time of posting the charge by use of the /Charges/Charge C (command) column options B, C, and Z.
Withhold Amount: This field is used to indicate either the actual dollar amount to be withheld or the percentage amount to be used to calculate the dollar amount to be withheld according to the contracted withhold. Leave this field blank if no withhold is required.
Adjustment Code: This field is used to indicate the /Utility/Messages/Remark <Remark Code> to be used as the desired withhold adjustment remark.
See CONTRACT EXAMPLE, Example 4,
The Stop Loss Amount field is informational only and may be left blank.
Stop Loss Amount: Enter the Stop Loss Amount.
The Insurance Code field MUST BE ENTERED WHEN A FEE SCHEDULE IS USED.
Insurance Code: Enter the /Utility/Insurance <Insurance Co. Code> field entry which indicates the entries within the fee schedule to use.
This field is used to determine which entries to use within the fee schedule specified in the Provider Code field below.
This field allows you to share, for example, the Medicare entry within a fee schedule with another insurance.
Normally, the Insurance Code field would be left blank for contracts based on a conversion rate/unit value contractual agreement. The exception would be when a specific procedure is negotiated as fee for service.
When this happens, set up a fee schedule for the appropriate provider containing the insurance and fee for service charge(s). Enter the /Utility/Insurance <Insurance Co. Code> field entry for the insurance company in this field. This indicates that although this pay plan is based on a conversion rate/unit value agreement, the fee schedule of the provider indicated in the Provider Code field below contains fee for service charge(s). Be sure to appropriately flag the /Utility/Procedure <HMO Adjust> field and/or use the pay plan Carve Out field above. For additional information for HMO Adjust, see Session II’s /Utility/procedure section regarding the field HMO Adjust and/or Software Requirements for Capitated (Pre-Paid) Contract Set Up.
The Provider Code field would contain an entry when sharing another provider’s fee schedule. Leaving this field blank indicates to On-Staff to use the fee schedule of the provider to which charges are posted for the above noted Insurance Code field entry(ies) within the fee schedule.
Provider Code: Enter the /Utility/Procedure/Fee Schedule <Provider Code> field entry for the provider whose fee schedule is to be used. If this field is left blank, the fee schedule of the provider to which charges are posted will be used.
The Provider Code field would normally be left blank for conversion rate/unit value contractual agreements. The exception would be when a specific procedure is negotiated as fee for service. See the Insurance Code field above.
See CONTRACT EXAMPLE, Example 5,
The Days to Bill and Days to Pay fields are informational only and may be left blank.
Days to Bill: Enter the maximum number of days allowed by this plan to bill out charges.
Days to Pay: Enter the maximum number of days this plan is allowed to make payment in.
The Allowable (R/F/N) and Multiplier fields will be used ONLY AFTER the fee schedule is checked and it is determined that the approved amount does not exist for the charge.
Allowable (R/F/N): This field is used to determine the approved amount. Press the [F2] search key to display the following valid choices:
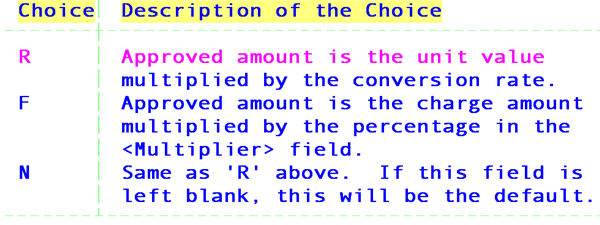
Multiplier: Enter the percentage to multiply the charge by to get the approved amount.
See CONTRACT EXAMPLES, Example 6,
The following Authorization Phone through Comment fields are for general information and may be left blank.
Authorization
Phone: Enter the phone # for obtaining treatment authorizations.
Eligibility Phone: Enter the phone # for obtaining eligibility information.
Comment: Enter any comments you may have regarding this plan. This field is 2 lines.
Related screens and fields:
/Utility/…/Pay Plan/Procedure
/Utility/…/Pay Plan/Diagnosis
/Utility/Procedure/Fee Schedule
/Utility/Procedure/Unit
CONTRACT EXAMPLES
Example 1: Carve Out
1A) Carve out the specified procedure(s).
A particular capitated contract states that injections and electrocardiograms will be paid as fee for service. Therefore, payment will be made on a separate check and will be carved out of, or excluded from, the monthly cap check.
Enter P in the Carve Out field and enter the injection and electrocardiogram procedures in the /Utility/Insurance/Pay Plan/Procedure screen for this pay plan.
/Pay Plan/Pay Plan field:
Phone : Carve Out : P
1B) Carve out the specified diagnosis.
A particular capitated contract states that whenever the diagnosis Renal Failure is posted, all related charges will be paid as fee for service. Therefore, payment will be made on a separate check and will be carved out of, or excluded from, the monthly cap check. Normally, some of these charges would have been included in the monthly cap check.
Enter D in the Carve Out field and enter the diagnosis code in the /Utility/Insurance/Pay Plan/Diagnosis screen for the pay plan.
/Pay Plan/Pay Plan field:
Phone : Carve Out : D
1C)
Carve out the specified procedure(s) and diagnosis.
A particular capitated contract states that whenever injections and electrocardiograms as well as the diagnosis of Renal Failure is posted, all related charges will be paid as fee for service. Therefore, payment will be made on a separate check and will be carved out of, or excluded from, the monthly cap check. Normally, some of these charges would have been included in the monthly cap check.
Enter B in Carve Out field. Enter the injection and electrocardiogram procedures in the /Utility/Insurance/Pay Plan/Procedure screen for this pay plan. Enter the diagnosis code in the /Utility/Insurance/Pay Plan/Diagnosis screen for the pay plan.
/Pay Plan/Pay Plan field:
Phone : Carve Out : B
Example 2: Conversion 0 (1, 2, 3, 4) and Percent fields.
2A) Conversion rate/unit value based contracts vary from one insurance contract to another. These contracts may be accommodated by setting up different pay plans and associating them with particular conversion rates and unit values. For example, a contract's conversion rate for ‘medical’ procedures (/Utility/Procedure <Type of Service> = 01) is 6.15. The Conversion 1 field is selected to be used for medical conversion rates (/Utility/Procedure <Conversion> = 1). Using the following panel code 99213 whose charge global Unit Value is 5.2, On-Staff will:
· Multiply the conversion rate (6.15) by the unit value (5.2) to get the Open Item Payment Approved amount of $31.98.
· Multiply the approved amount ($31.98) by the percent (80) to get the insurance reimbursement of $25.58 (Open Item Payment Method A).
· Subtract the approved amount ($31.98) from the charge global ($50.00) to get the contract adjustment of $18.02 (Open Item Payment Method A).
· Subtract the insurance reimbursement ($25.98) from the approved amount ($31.98) to get the Charge screen’s <Patient> balance of $6.40.
/Pay Plan fields:
Conversion 1 : 6.15 Percent: 80.00
2B) Fee schedule based contracts (e.g., some HMO or IPA contracts base their contract approved amounts on Medicare's fee schedule) may vary in the percentage of the approved amount they will pay. These contracts may now be accommodated by setting up different pay plans. ONLY the Percent fields would be completed for each type of procedure, leaving the Conversion 0 through Conversion 4 fields blank. Which Percent field is used is determined by the /Utility/Procedure <Conversion> field entry. The Conversion 1 field is selected to be used for medical contract rates (/Utility/Procedure <Conversion> = 1). Using the following /Utility/Procedure example, On-Staff will:
· Calculate the insurance reimbursement (Open Item Payment Method A) as 80% of the Fee Schedule Approved amount.
· Calculate the Charge screens’ <Patient> balance as 20% of the Fee Schedule Approved amount (or Approved minus insurance reimbursement).
/Pay Plan fields:
Conversion 1 : 0.00 è Percent: 80.00
Example 3: <Scale Code> and <Unit Value Pointer>.
3A) Scale Code and Unit Value Pointer of 1.
A particular insurance company uses the McGraw Hill scaling system (i.e., the /Utility/Procedure/Unit Value screen for <Scale Code> = MH) without variation. Enter the user-defined scale code MH for this scale in the Scale Code field and enter 1 in the Unit Value Pointer field to indicate the column the unit values are in.
/Pay Plan fields:
Scale Code : MH Unit Value Pointer : 1
3B) Scale Code with Unit Value Pointer of 2.
A particular insurance company uses the McGraw Hill scale, however, the practice has negotiated that the unit value for all office visits will be increased by 5% to allow for a higher reimbursement. In the Global 2 column, duplicate the Global 1 unit value for each procedure, except for each office visit, multiply the Global 1 unit value by 5% and enter this product in the Global 2 column. Enter the user defined scale code MH for this scale in the Scale Code field and enter 2 in the Unit Value Pointer field to indicate the column the unit values are in. /Pay Plan fields
:
Scale Code : MH Unit Value Pointer : 2
3C) Scale Code and Unit Value Pointer left blank.
A practice has determined that all their insurance contracts use the McGraw Hill scaling system and have entered the unit values in the appropriate /Utility/Procedure <Unit Value> fields.
NOTE: The unit value will be pulled from the appropriate /Utility/Procedure <Unit Value> field when:
· The Scale Code and Unit Value Pointer fields are not entered. See FIG. 1.
· The Scale Code and Unit Value Pointer are entered but:
a) there is no /Utility/Procedure/Unit Value screen for the indicated scale code.
b) the /Utility/Procedure/Unit Value screen exists for the indicated scale code, but there is no /Utility/Procedure/Unit Value <Global 1 (or 2, 3)> column entry for the indicated unit value pointer.
c) the /Utility/Procedure/Unit Value screen for the indicated scale code does not contain the procedure code being posted. See FIG. 2.
FIG. 1 /Pay Plan fields:
Scale Code : Unit Value Pointer :
Example 4: Withhold calculations.
The contract approved amount for a 99213 panel code is $31.98 (The appropriate pay plan conversion rate/unit value or fee schedule fields must be completed to calculate the approved amount). The insurance contract states that payment will be 80% of the approved amount, leaving an expected insurance reimbursement of $25.58 and a patient balance of $6.40. If this charge is subject to a 2% withhold, calculated on the approved amount of $31.98, the withhold will be $.63 ($31.98 x .02). The expected insurance reimbursement would be $25.08 ($31.98 x .80), leaving a withhold amount of $.63 being posted, leaving the same patient balance of $6.40.
/Pay Plan/Pay Plan fields:
Withhold (F/C/A/N) : A Withhold Amount : 2.00
Adjustment Code : IWA* Stop Loss Amount :
*This is a user defined remark code that must exist in the /Utility/Messages/Remark screen. IWA may be defined as Insurance Withhold Adjustment.
Example 5: Insurance Code and Provider Code
5A) You are a single physician practice. You have entered a fee schedule for Insurance Co. Code MCAR (Medicare's /Utility/Insurance <Insurance Co Code>) into the /Utility/Procedure/Fee Schedule screen for this provider. The following pay plan fields would then be set up.
/Pay Plan/Pay Plan fields:
Insurance Code : MCAR Provider Code :
You may want to share the Medicare fee schedule entry with other insurance companies whose contracts are based on Medicare's approved amounts. For example, you are entering a patient with Medicare/Medi-Cal insurance coverage or you have an HMO contract whose fee schedule is the same as Medicare's. By entering the Medicare pay plan code in the New Patient Insurance screen Pay Plan field, you are indicating to On-Staff to use or share the approved amounts and alternate charge amounts of the Medicare entry within the fee schedule. Therefore, adding identical entries within the fee schedule except for this other insurance company is not necessary. By leaving the Provider Code field blank, you are indicating to On-Staff to use the fee schedule of the provider the charges are being posted to.
When posting charges On-Staff will check the New Patient Insurance screen for a Pay Plan code. Next, On-Staff will obtain the Insurance Code field entry for this pay plan as well as the Charge screen Dr and Panel Code field entries, then look for the /Utility/Procedure/Fee Schedule entries for those codes. When found, On-Staff will post the fee schedule’s Alternate column entry as the charge amount. When not found, On-Staff will then look for a pay plan Procedure Code entry and check that fee schedule as previously noted. When not found, On-Staff will post the /Utility/Procedure <Charge Global> field entry as the charge amount.
5B) When a practice consists of several physicians and contracts are obtained as a group, all physicians in the clinic would then use the same fee schedule(s). You would set up multiple pay plans, one for each contract. You would set up all the fee schedule contracts under one provider, then share this set up with the others. The following pay plan fields would then be entered:
/Pay Plan/Pay Plan fields:
Insurance Code : MCAR Provider Code : 1
Insurance Code : MM Provider Code : 1
Insurance Code : HMO Provider Code : 1
By entering the pay plan code in the New Patient Insurance screen Pay Plan field, you are indicating to On-Staff to use or share the approved amounts and alternate charge amounts of the fee schedule for the indicated Insurance Code entries within the fee schedule for the indicated Provider Code> The indicated Insurance Code fee schedule entry must exist in that fee schedule. Setting up pay plans to share in this way thus relieves you of the task of entering a separate fee schedule into the /Utility/Procedure/Fee Schedule area for each provider and each contract's insurance company code.
When posting charges On-Staff will check the New Patient Insurance screen for a Pay Plan code. Next, On-Staff will obtain the Insurance Code field entry and Provider Code field entry for this pay plan as well as the Charge screen Panel Code field entries then look for the /Utility/Procedure/Fee Schedule entries for those codes. When found, On-Staff will post the fee schedule's Alternate column entry as the charge amount. When not found, On-Staff will post the /Utility/Procedure <Charge Global> field entry as the charge amount.
5C) You have a conversion rate/unit value based contract where specific procedures were negotiated as fee for service and you want to set up those procedures’ contracted approved amounts. For example, your Gateway pre-paid (capitated) contract states that whenever an injection for Lupron is billed it has a contract approved amount of $235.00 To handle this contractual agreement, you would enter P on the pay plan Carve Out field and enter the procedure in the /Utility/Insurance/Pay Plan/Procedure screen for this pay plan. You would next enter the appropriate code in the pay plan Insurance Code and Provider Code fields as well as enter the contract approved amount information in the /Utility/Procedure/Fee Schedule for the Lupron charge.
Example 6:
For example, you have determined what the usual and customary fees are for your area and have entered these on the /Utility/Procedure <Charge Global> field. A contract with a carrier approves 70% of the charge and pays 80% of the approved amount.
/Pay Plan/Pay Plan fields:
Conversion 0 : Percent : 80
Conversion 1 : Percent : 80
Conversion 2 : Percent : 80
Conversion 3 : Percent : 80
Conversion 4 : Percent : 80
Scale Code : Unit Value Pointer :
Withhold (F/C/A/N) : Withhold Amount :
Adjustment Code : Stop Loss Amount :
Insurance Code : Provider Code :
Days to Bill : Days to Pay :
Allowable (R/F/N) : F Multiplier : 70