
OnSTAFF 2000
Charges /UB Encounter/Add.
General Information Regarding Encounter Screens
There are three types of encounter screens: Encounter, Worker’s Comp Encounter and UB Encounter. These screens serve several purposes. They allow entry of additional claim information such as authorization numbers, information for attorney, lien or worker's comp cases, hospital admission and discharge dates and more. This information is stored for later retrieval.
Encounters:
When the patient has an insurance category type, an encounter may be added, modified or viewed through Main Menu/New Patient/Add, Modify or View.
NOTE: Main Menu/New Patient/Add allows adding encounter information upon registering a new patient. After exiting the Add New Patient mode, encounters may only be added through Main Menu/Charges /Encounter/Add.
Independent of the patient’s category type, an encounter may be added, modified, viewed or deleted through Main Menu/Charges/Encounter/Add, Modify, View or Delete.
Worker’s Comp Encounters:
When the patient has a worker’s comp category type, a worker’s comp encounter may be accessed only through Main Menu/New Patient/Add, Modify or View.
UB Encounters:
Independent of the patient’s category type, UB encounters may only be added, modified, viewed or deleted through Main Menu/Charges/UB Encounter/Add/Modify/View or Delete.
See NOTE regarding category types.
.
UB Encounter Information
Independent of the patient’s category type, UB encounters may only be added, modified, viewed or deleted through Main Menu/Charges/UB Encounter/Add, Modify, View and Delete. When UB Encounter is selected from the Charge Menu, On-Staff will display the following:

When the Add option is selected, On-Staff will display the following:
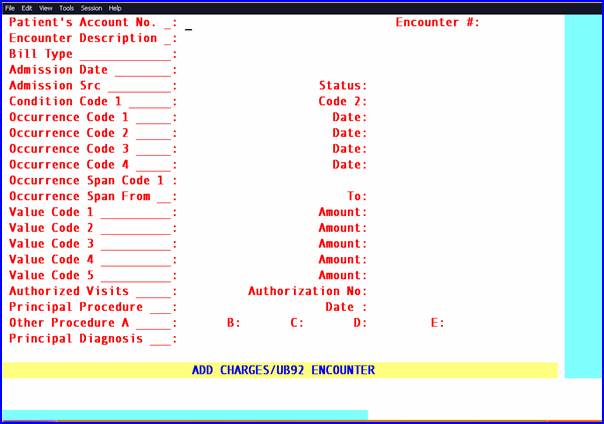
Patient’s
Account No.: When not already displayed, enter the patient’s account number. When the account number is unknown, enter all or part of the name (last name, first name format) and/or incorporate the Wild Card (*) then press the [F2] search key.
Encounter #: This number is assigned automatically when adding a new record. When this information is modified later, the number of each encounter may be retrieved individually. When the encounter number is unknown, clear the field by pressing the [Spacebar] then press the [F2] search key to display
the Selection Screen for Claim. When [F2] is pressed again, ALL encounters entered for that patient will be displayed. To select an encounter, move the cursor to highlight the desired one and press [Enter]. To exit this screen without making a selection , from the C (command) column press Q or [End].
Encounter
Description: Does not print on claims, but may be useful when using [F2] search to find encounters.
Bill Type: Enter a valid Bill Type code. This must be 4 digits, first digit is a leading zero Will complete TYPE OF BILL box 4 CMS 1450 (UB-04) with this code. This is required for Medicaid billing. The type of bill code includes the two-digit facility type code and one-character claim frequency code. This is a required field when billing Medi-Cal
Admission date: Prints in Box 12 of the UB form.
Or electronic claims submission Loop 2300 DTP *435*D8*.
Admission Src: Type the appropriate Source of Admission code. View Source Codes.
This code prints in Box 15 of the UB form.
Claims will be rejected if the <Admission Src> field is not filled-out with the appropriate codes based on your billing requirements.
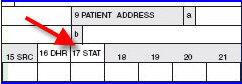
Status: Type the hospital discharge status code indicating patient’s disposition as of the ending date of service. View Patient Discharge Status Codes
Prints in Box 17 of the UB form.
Claims will be rejected if the <Status> field is not filled-out with the appropriate codes based on your billing requirements.
Or electronic claims submission Loop 2300 CL1*.
Code 1: Type a valid condition code. Required entry. View Condition Codes
Prints in Box 18 of the UB form.
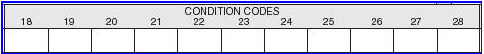
Or electronic claims submission Loop 2300 HI*BG:
Code 2: Prints in Box 19 of the UB form.
GUIDELINES FOR OCCURRENCE AND OCCURRENCE SPAN UTILIZATION
Code 1 / Date: Type a valid occurrence code. View Occurrence Codes
Prints in Box 31 of the UB form.
Or electronic claims submission Loop 2300 HI*BH:
Occurrence
Code 2 / Date: Prints in Box 32 of the UB form.
Occurrence
Code 3 / Date: Prints in Box 33 of the UB form.
Occurrence
Code 4 / Date: Prints in Box 34 of the UB form.
Span From / To: Prints in Box 35 of the UB form along with Occurrence Span Code 1.
Or electronic claims submission Loop 2300 HI*BI:
/ Amount: Will complete VALUE CODES CODE box 39a CMS 1450 (UB-04).
Or electronic claims submission Loop 2300 HI*BE:
Value Code 2
/ Amount: Prints in Box 40a of the UB form.
Value Code 3
/ Amount: Prints in Box 41a of the UB form.
Value Code 4
/ Amount: Prints in Box 39b of the UB form.
Authorization Enter the authorization number issued by private insurance companies (i.e., an HMO tar
No.: number) for treatment given under this encounter. This information will print in Box 63 of the UB form and will be transmitted electronically for all insurance types other than Medi-Cal (Utility/Insurance <Insurance Type> does not equal D).
Authorized No.
of Visit: Enter the number of visits the insurance company authorized for treatment under this encounter. This field will decrement the number for each unique service date as charges are posted to this encounter. When the encounter number is entered on the Charge Screen and [Enter] has been pressed, the number of remaining authorized visits will be displayed. Only whole numbers should be used (i.e., 1, 2, 10). This field will accept numbers such as 10.30 but the .30 will not be recognized.
Procedure: Enter the actual CPT Code (i.e., the surgeons code for hospital billing).
Will complete PRINCIPAL PROCEDURE CODE box 74 CMS 1450 (UB-04).
Or electronic claims submission Loop 2300 HI*BR:
Date: Type the DOS for the Principal Procedure. Will complete PRINCIPAL PROCEDURE DATE and OTHER PROCEDURE DATE box 74 a- e CMS 1450 (UB-04).
Other
Procedure: Type any other CPT code for this encounter.
Diagnosis: Type the most specific ICD-9 (up to five digits) code describing the principal diagnosis (e.g., the condition established after study to be chiefly responsible for causing the admission or other health care episode). Do not enter manifestation codes as the principal diagnosis; code the underlying disease first.
1. For inpatient claims: The principal diagnosis selected must be the reason for admission. It should relate to one or more conditions or symptoms identified in the admission notes and/or admission work-up. Manifestation codes are not to be recorded as the principal diagnosis; code the underlying disease first. The principal diagnosis code may not include “E” codes. “V” codes may be used as the principal diagnosis.
1. For outpatient claims: The principal diagnosis identifies the condition chiefly responsible for the patient’s visit or treatment. The principal diagnosis code may not include “E” codes. “V” codes may be used as the principal diagnosis
Will complete box 67 CMS 1450 (UB-04).

Or electronic claims submission Loop 2300 HI*BK:
NOTE: Principal Procedure and Date are not transmitted when billing electronically.
After the last field has been entered, the cursor will return to the Encounter Description field allowing the user to review the accuracy of the entered data. When accurate, to exit this process press [“] or [End]. Refer to the section UB REVIEW, included in Session III, for additional per box, form information.