
OnSTAFF 2000
hapter 4 MAIN MENU/UTILITY/
INSURANCE MENU
This option is used in adding to and maintaining insurance companies for billing purposes and contains contractual information (/Pay Plan) and electronic billing requirements (/Tele Com) and more. Standard to On-Staff are numerous pre-entered Insurance screens as well as partially set up Tele Com screens. The partially completed Tele Com screens are for MCAR (Medicare), MM (Medi-Medi), MCAL (Medical) and IMS (ProxyMed/IMS) Insurance Co. Codes.
Menu Options:
Add Add an Insurance Company.
Modify Modify an existing Insurance Company.
Delete Delete an existing Insurance Company.
View View an existing Insurance Company.
Print Prints a list of Insurance Companies.
Tele Com Set up for electronic billing.
Pay Plan Contractual information.
Search Search screen (see Session II index).
Exit Returns you to the Utility Menu.
REMINDER:
Regarding Selection Screen for Insurance search screens, pressing the [F2] search key on a blank Selection Screen for Insurance is requesting On-Staff to pull the complete library, ALL insurances. This library is quite extensive, thus you will be waiting awhile for this information to be pulled into your search screen. From the C (command) column of the Selection Screen for Insurance you may Add, Modify, Inquire and Delete as desired. On-Staff will not allow the deletion of an entry if that entry has been selected for use within the On-Staff program. Pressing [Enter] will default the highlighted entry into the field from which you pressed [F2].
/Utility/INSURANCE/Add, Modify, View, Delete
The Add, Modify, View and Delete options maintain Insurance setup, allowing you to Add new, Modify or View existing and Delete Insurance Codes entered in error.
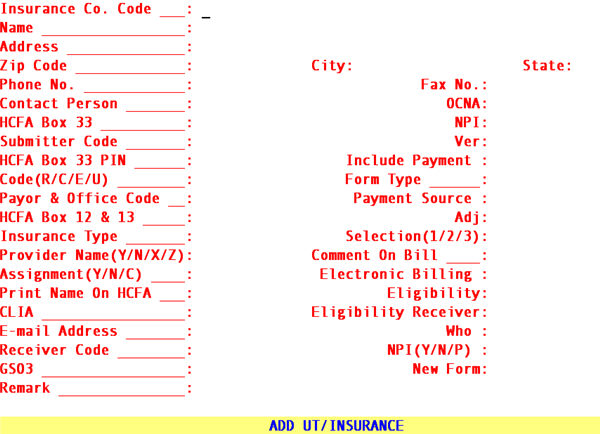
To add an insurance company, select the Add option and On-Staff will display the following fields:
NOTE: Various fields of the Add New Insurance screen will contain values defaulted there from the Insurance Co. Code DEF. Your trainer will assist you in the set up of insurance DEF . Keep in mind, when adding a new Insurance you MUST determine, for fields that do not default a value, what value should be entered (if any).
Insurance Co.
Code: Enter up to 6 characters of letters and/or numbers. For example, for the first Aetna entry, you may want to use AET001. This code will allow you to set up 999 Aetna entries/records with different addresses.
NOTE It is not an issue to be able to remember the Insurance Co. Code. Using
On-Staff's [F2] search key feature, allows the user to search by the name of the insurance company. On-Staff does not automatically assign the next available Insurance Co. Code. That code is user defined.
Name: Enter the name of the Insurance company.
Address: Enter the address of the Insurance company.
Zip Code: Enter the zip code of the Insurance company.
City: Displayed automatically if the zip code is known to On-Staff; otherwise enter the city attached to the zip code.
State: Displayed automatically if the zip code is known to On-Staff; otherwise enter the state attached to the zip code.
Phone No.: Enter the phone number of the insurance company.
Fax No.: Enter the fax number of the insurance company, if applicable.
Contact Person: Enter the name of the contact person if applicable.
OCNA: Used to identify the crossover carrier for Medicare. If the Medicare intermediary crosses over to private Medi-Gap carriers, enter the applicable code in this field. Medicare will then automatically forward claims to the appropriate carrier. These are now COBA codes which are obtained from Medicare.
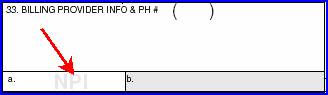
HCFA Box 33: Enter the group number assigned to your practice by this insurance carrier. This field WILL PRINT in Box 33 of the HCFA 1500 claim form ONLY WHEN BILLING METHOD IS BY CLINIC. When billing method is by Doctor, leave this field blank.
NOTE: When the billing method is by CLINIC*:
/Utility/Set Up/Parameter <Billing> = C. If this field is left blank, then
/Utility/Category <Billing (D/C/N)> = C.
When billing method is by DOCTOR*:
/Utility/Set Up/Parameter <Billing> = D. If this field is left blank, then /Utility/Category <Billing (D/C/N)> = D.
*Billing methods were determined during Session I.
NPI Type the Group NPI if applicable.
If Provider Facility or Provider Provider do not meet the billing criteria and if <Billing Method> = “C” then System will complete this code in CMS1500 Box 33a.
Submitter Code: Each carrier to which you submit electronic claims directly will assign you a submitter code. Enter the submitter code assigned by the carrier. Provided by On-Staff are the following Insurance Co. Codes for carriers accepting electronic claims, the most common listed first:
HCFA 1500 claim form electronic billing:
MCAR Medicare
Northern California:
Enter the UIC# assigned by CABBS.
Southern California:
This code MUST BE NINE DIGITS LONG, thus you may need to add leading zeros (not capital o's) i.e., Medicare assigns 3008 as your submitter code. You would then enter 000003008 on the Submitter Code field.
MM Medicare/Medi-Cal Crossover
Northern California:
Enter the UIC# assigned by CABBS.
Southern California:
This code MUST BE NINE DIGITS LONG, thus you may need to add leading zeros (not capital o's) i.e., Medicare assigns 3008 as your submitter code. You would then enter 000003008 on the Submitter Code field.
IMS Integrated Medical Systems.
Enter your three character code assigned by IMS.
MCAL Enter your three digit code assigned by Medi-Cal.
HPSM Health Plan of San Mateo
a Medi-Cal Intermediary in Northern California
NAMM North American Medical Management
a Medicare Intermediary for IPA’s in Northern California
DDD Diversified Data Design
Covers Cigna HMO for Southern California, United Health Plan HMO, Maxicare HMO and Care First HMO.
UB04 form electronic billing:
UGS United Government Services
MCAR-A Blue Cross Medicare Part A
Note (November 2011): For clients sending ANSI 5010 claims to OptumInsight (formerly Ingenix/ENS), enter ZLI#(GS-02).
NOTE: You may electronically submit the following types of claims:
MSP (Medicare as a secondary payor)*
MSP and MG (Medicare as secondary payor and a Medigap Supplement)* Anesthesiology
Chiropractic
Podiatry.
Ambulance.
* Although these may be submitted electronically, these carriers require the primary insurance EOB which at this point in time is not able to be transmitted with the claim, thus paper billing is required
Ver: This field will default to 00104. This field has been set appropriately for all Insurances provided by On-Staff. Pressing the [F2] search key will display the following valid choices:
CHOICE DESCRIPTION OF CHOICE
00104 ALL carriers but the following EXCEPTION:
00200 Medicare .
Effective version 8.2 10/06/2011, the version for sending claims in ANSI 5010 format must be updated to the new version number. See below for the appropriate version number based on the type of billing your office transmits:
• Part B Version (Professional/HCFA): The version number has changed from 004010X098 to 00501.
• Part A Version (Institutional/UB): The version number has changed from 004010X096 to 00501.
Please remember: These codes must be used after January 1, 2012, but DO NOT change the version number until you are ready to send 5010!
HCFA
Box 33 PIN For Medi-Cal ONLY (Insurance Co. Code MCAL). Enter your seven digit eligibility verification number assigned by Medi-Cal. This will print on the PIN# portion of Box 33 on the HCFA 1500 form.
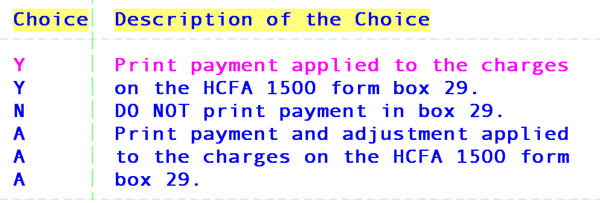
Payment: This field allows you to specify if this insurance will print a dollar amount in Box 29 of the HCFA 1500 and/or UB92 claim forms. This field has been set to N for all Insurances provided by On-Staff. Inform your trainer if you want this changed. Press the [F2] search key to display the following valid choices:
Code (R/C/E/U): For Insurances provided by On-Staff, this field has been set to use the coding from /Utility/Procedure as follows, inform your trainer if you want this changed:
R Use the /Utility/Procedure Code R coding system for this carrier. (Usually for Medi-Cal).
C Use the /Utility/Procedure Code C coding system for this carrier. (Usually for ALL carriers BUT Medi-Cal and Medicare).
E Use the /Utility/Procedure Code E coding system for this carrier. (Usually for Medicare, Medi-Medi and ANY other carrier accepting HCPCs).
U Use the /Utility/Procedure UB92 Code coding system for this carrier.
When adding a new insurance, choose the method of coding from /Utility/Procedure appropriate for this insurance company.
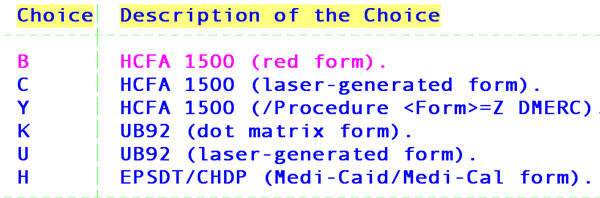
Form Type: For Insurances provided by On-Staff, this field has been set to C for all carriers except for Medicare, Medi-Medi and Medi-Cal which are B. Inform your trainer if you want this changed.
When adding a new insurance, choose the type of insurance form to be printed for this insurance company. Press the [F2] search key to display the following valid choices:
Code: Used for electronic billing. ONLY the following carriers require an entry.
Note (November 2011): For clients sending ANSI 5010 claims to OptumInsight (formerly Ingenix/ENS), enter INGENIX (ISA-08).
Payment Source: This field has been set for Insurances provided by On-Staff.
When adding a new insurance, enter the /Utility/Messages/Remark <Remark Code> that best describes a payment received from this insurance company.
Box 12 & 13 This is the message that prints on boxes 12 and 13 of the HCFA 1500 claim form.
This field has been set to read SIGNATURE ON FILE for Insurances provided by On-Staff and is recommended that you do the same when adding a new insurance.
Adj: This field has been set for Insurances provided by On-Staff.
When adding a new insurance Enter the /Utility/Messages/Remark <Remark Code> that best describes an adjustment received from this insurance company.
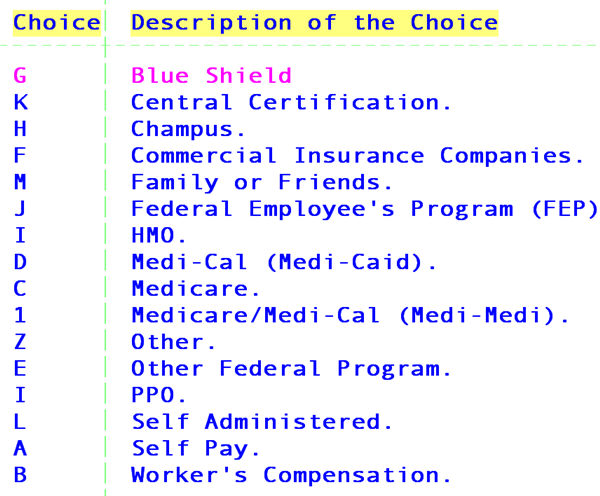
Type: Press [F2] and select the appropriate insurance type by moving the cursor to highlight that type and press [Enter]. It is important for electronic billing that the correct Type is assigned to each carrier. Valid choices are:
(1/2/3): Entering a 1, 2 or 3 will determine which, provider number (/Utility/Provider <Provider No. 1 (2 or 3)> for BOTH billing methods) group number (/Utility/Provider <Group No. 1 (2 or 3)> for billing method by Doctor ONLY) place of service code (/Utility/Facility <Place of Service 1 (2 or 3)>) and facility provider number (/Utility/Facility <Provider 1 (2 or 3)>) will appear on the claim form. This field has been set for Insurances provided by On-Staff as follows:
1 ALL carriers but the following exceptions.
2 Blue Shield.
3 Champus, Connecticut General and Cigna.
Your trainer will advise you if your set up requirements are different.
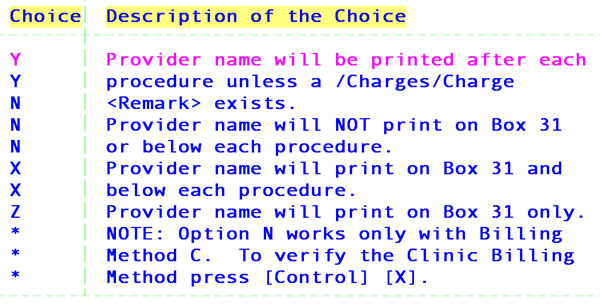
(Y/N/X/Z): This field sets where and if the provider's name is to be printed on the HCFA 1500 claim form. This field has been set to Z for Insurances provided by On-Staff. Inform your trainer if you want this changed. Press the [F2] search key to display the following valid choices:
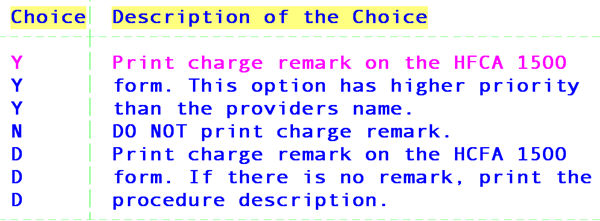
Bill: This field allows the ability of printing a remark or procedure description on the HCFA 1500 claim form. This field has been set to Y for Insurances provided by On-Staff. Inform your trainer if you want this changed. Press the [F2] search key to display the following valid choices:
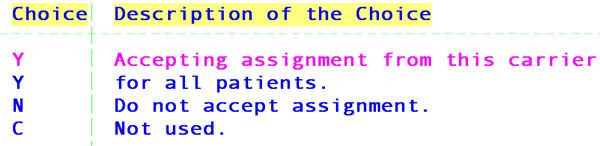
(Y/N/C): This field indicates whether or not your clinic accepts assignment with this particular insurance company. Y will mark the YES Box on Box 27 of the HCFA 1500 claim form. N will mark the NO box. This then eliminates the data entry staff from having to determine whether or not assignment is accepted. This field has been set to Y for all Insurances provided by On-Staff. Inform your trainer if you want this changed. Press the [F2] search key to display the following valid choices:
Billing: This field will specify which electronic billing module will be used (if applicable). This field has been set for Insurances provided by On-Staff for carriers accepting electronic claims through IMS to I, for Insurance Co. Codes MCAR and MM to M, Insurance Co. Code MCAL to S.
On HCFA: This field allows you to specific if this insurance will print the name and address in the upper right hand corner of the HCFA 1500 claim form or in Box 38 of the UB form.
CMS 1500

UB04

Press the [F2] search key to display the following valid choices:
Y Print Name of the Insurance.
N Do Not Print Name of Insurance.
Eligibility Not Used
CLIA: This field allows you to specify if this insurance will print the CLIA number located on the /Utility/Provider <CLIA> field in Box 23 of the HCFA 1500 claim form or send electronically. Press the [F2] search key to display the following valid choices:
Y Print the CLIA# or submit it electronically for this carrier.
N Do NOT print the CLIA# or submit it electronically.
Eligibility Receiver Not Used
E-mail Address: Enter their E-mail address. This is an informational field only and will not print anywhere.
Who: This field allows you to specify who is responsible for payment after primary payment is received regardless if there is a secondary insurance or not. For example, if this field is set to G, if the patient has both a primary and secondary insurance entered and the patient’s assigned category <Responsibility (G/P/X)>is set to P, after their primary insurance payment has been posted, their ledger W (who) column will change to G denoting the Guarantor/Patient is responsible for payment on any remaining balance (not S secondary insurance responsibility). This will give you the advantage of sending a statement after primary carrier payment is received and still bill the secondary. Press the [F2] search key to display the following valid choices:
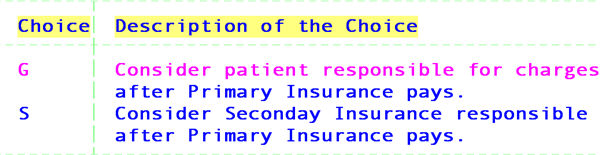
NOTE: If this field is set to G the W (who) column will change to G after primary payment is posted, hence you will not be able to use R (rebill) in the /Billing/Insurance <All/Unbill/Rebill (A/U/R/H)> field. Instead, enter A in this field and S (secondary carrier) in the /Billing/Insurance <Primary/Sec/All (P/S/A)> field.
Receiver Code Used for electronic claims submission. Type the Payer Id provided by the electronic claims carrier or clearinghouse.
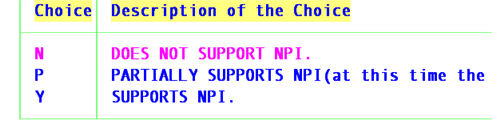
NPI
(Y/N/P) Used to determine electronic claims submission. If carrier accepts NPI, enter “Y” yes.
Press the [F2] search key to display the following valid choices:
GS03 Electronic claims submission. The Application Receiver’s Code in GS03 can be used to identify the receiving unit of the transmission. For health care, this unit identification >can be used to differentiate between managed care, indemnity, and Medicare. Identification code published by the functional group receiver (sent in GS02 of the 270 interchange inquiry) for other parties to use as the receiver ID to route data to them.
Note (November 2011): For clients sending ANSI 5010 claims to OptumInsight (formerly Ingenix/ENS), enter INGENIX.
New Form Enter“Y” for the CMS1500 (08-05) and the UB-04 with NPI and legacy identifiers or “X” only NPI, excluding the legacy identifiers, or ‘N’ to continue printing on the CMS 1500 (10-93) and UB04.
Remark: This is an informational field and is for your eyes only. Enter up to two lines of remarks about this insurance company.
After pressing [Enter] in the last field, the cursor will return to the Name field, allowing review of the entry for accuracy. If the data entered is accurate, press [“] to return to the Insurance Co. Code field. At this point, you may either add an additional insurance company or press [“] to return to the Insurance Menu.
DO NOT DELETE THE FOLLOWING INSURANCE CO. CODES provided by On-Staff: IMS, CASH, CPAY and GUR. These came with your system. DO NOT DELETE THEM! If for
some reason they do not exist, please add them, duplicating the following screens. ONLY the highlighted fields require information. The remaining fields may be left blank. For CPAY and GUR insurance screens, the fields Payment Source and Adj. (see *) require the /Utility/Messages/Remark <Remark Code> that describes a patient payment and/or a patient co-payment.
Insurance Co. Code : IMS
Name : IMS CLEARING HOUSE
Address :
Zip Code : City : State:
Phone No. : ( ) ‑ Fax No.: ( )
Contact Person : OCNA :
Provider No. :
Submitter Code : your submitter code assigned by IMS Ver : 00104
Pin Number : Include Payment :
Code (R/C/E/U) : Form Type :
Payor & Office Code : Payment Source :
Message : Adj :
Insurance Type : Selection(1/2/3) :
Provider Name(Y/N/X/Z) : Comment On Bill :
Assignment(Y/N/C) : Electronic Billing : I
Print Name On HCFA :
CLIA : Who :
Remark :
MODIFY INSURANCE
Insurance Co. Code : CASH (and one for CPAY and GUR)
Name : CASH PATIENT (see previous paragraph for names)
Address :
Zip Code : City : State:
Phone No. : ( ) ‑ Fax No.: ( )
Contact Person : OCNA :
Provider No. :
Submitter Code : Ver :
Pin Number : Include Payment :
Code (R/C/E/U) : Form Type :
Payor & Office Code : *Payment Source :
Message : *Adj :
Insurance Type : Selection(1/2/3) :
Provider Name(Y/N/X/Z) : Comment On Bill :
Assignment(Y/N/C) : Electronic Billing :
Print Name On HCFA :
CLIA : Who :
Remark :