
Intellect™
BILLING MENU OPTIONS

Insurance
Pre-Billing Report
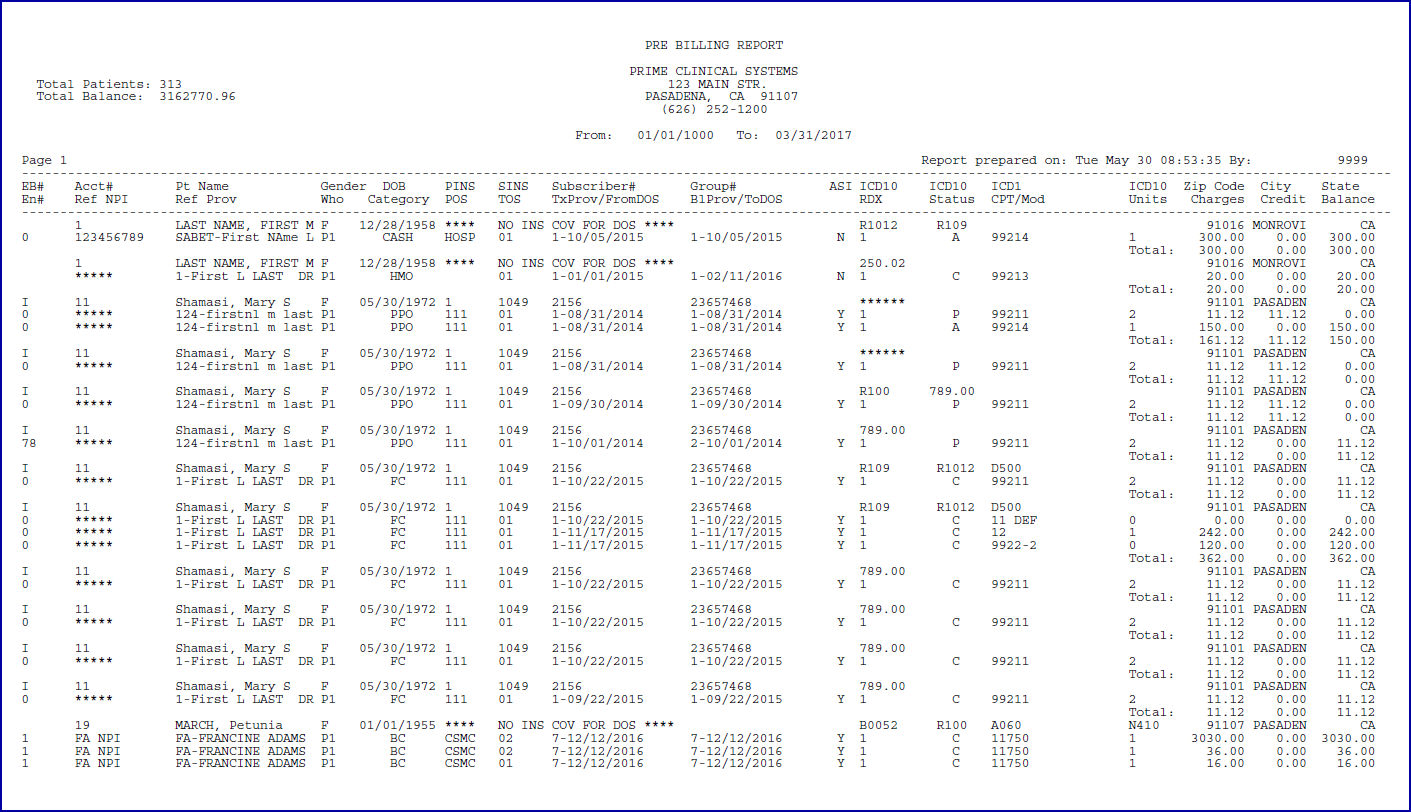
Sample Pre-Billing Report
The pre-billing report is generated via Billing --► Insurance --► Group of Patients by selecting 'PRE BILLING REPORT' in the <Form Type> field. For other required settings in Billing --►Insurance --►Group of Patients, see Pre-Billing Report. Additionally, a review of the various column headings follows the samples below.
Effective Version 17.06.09 - ICD9 headings changed to ICD10
Effective Version 9.12.16
Versions prior to 9.12.16
There are 2 rows of column headings on the Pre-Billing Report.
• The column headings on the top line include: EB#, Acct#, Pt Name, Gender, DOB, PINS, SINS, Subscriber#, Group #, ICD10, Zip Code, City, and State.
• The column headings on the bottom line include: EN#, Ref NPI, Ref Prov, Who, Category, POS, TOS, TxProv/From DOS, BlProv/ToDOS, ASI, RDX, Status, CPT/Mod, Units, Charges, Credit, and Balance.
Definitions follow for each of the column headings.
I - Column Headings on the Top Line
II - Column Headings on the Bottom Line
I - Column Headings on the Top Line (from left to right)
The top line contains the demographic and insurance information for each account, along with the diagnosis codes linked to the charges on the lines below.
1. EB#
1.1 Displays the <Electronic Billing> field from the Utility --► Insurance --► Insurance screen for the patient’s primary insurance to indicate whether the insurance is set up for electronic submission and through which carrier type.
1.2 The most common Carrier Type codes are:
• ‘M’ for Medicare direct
• ‘I’ for clearinghouse
• ‘X’ for Medi-Cal/Medicaid direct
• (blank) for paper claims.
NOTE: The settings may differ if billing to more than one clearinghouse (or direct carrier) and/or for both professional and institutional claims.
1.3 If electronic billing setup needs to be confirmed or updated, see the Utility --► Insurance--► Insurance <Insurance Co. Code> for the primary insurance in 6 below and for the secondary insurance in 7 below.
1.4 IMPORTANT: If the Utility --► Insurance --► Insurance <Electronic Billing> field is NOT blank, a valid payer ID# must be entered in the <Receiver>, <Payer Identifier>, and <Payor & Office Code> fields.
2. Acct#
2.1 Displays the patient’s <Patient Account No> from the Registration --► Regular --► Patient OR Registration --► Worker --► Worker.
3. Pt Name
3.1 Displays the patient’s full name (<Last Name>, <First Name> <Middle Initial>) from the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen.
4. Gender
4.1 Displays the patient’s <Gender> from the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen.
4.2 This field is mandatory for billing.
4.3 If asterisks (*) appear in this column, electronic billing edits prevent electronic claim submission until the missing information is entered.
5. DOB
5.1 Displays the patient’s date of birth (formatted as MM/DD/YYYY) from the <DOB> field on the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen.
5.2 This field is mandatory for billing.
5.3 If asterisks (*) appear in this column, electronic billing edits prevent electronic claim submission until the missing information is entered.
6.1 The Primary Insurance column displays the Utility --► Insurance --► Insurance <Insurance Co Code> associated with the charge(s) as the patient’s primary insurance. NOTE: A Regular Patient Insurance or Worker Insurance screen must exist for this insurance code on the patient’s account.
6.2 ‘**** NO INS COV FOR DOS ***’ indicates there is no insurance coverage for the date of service when:
6.2.1 The patient is a ‘CASH’ patient with no insurance coverage.
- OR -
6.2.2 The date of service is NOT within the <Coverage From> and <Coverage To> range of the patient’s primary insurance(s) on the Regular Patient Insurance or Worker Insurance screen.
- OR -
6.2.3 The primary insurance was not entered at the time of charge posting.
6.3 The primary insurance associated with the charge(s) may be updated in the <Primary*> field on the Charges --► Modify [Information] screen. NOTE: When a new insurance screen is added to the patient’s account, the insurance code associated with previously posted charges does NOT change.
7.1 The Secondary Insurance column:
7.1.1 Displays the Utility --► Insurance --► Insurance <Insurance Co Code> associated with the charge(s) as the patient’s secondary insurance. NOTE: A Regular Patient Insurance or Worker Insurance screen must exist for this insurance code on the patient’s account.
- OR -
7.1.2 This is blank if no secondary insurance associated with the charge(s).
- OR -
7.1.3 Displays ‘**** NO INS COV FOR DOS ***’ when there is no primary insurance.
7.2 The secondary insurance associated with the charge may be updated in the <Secondary*> field on the Charges --► Modify [Information] screen. NOTE: When a new insurance screen is added to the patient’s account, the insurance code associated with previously posted charges does NOT change.
8. Subscriber#
8.1 Displays the patient’s primary insurance <Subscriber No.> from the Regular Patient Insurance or Worker Insurance screen. (See 6 above).
8.2 ‘**** NO INS COV FOR DOS ***’ is displayed when there is no primary insurance linked to the charge(s).
9. Group #
9.1 Displays the patient’s primary insurance <Group No.> from the Regular Patient Insurance or Worker Insurance screen. (See 6 above).
9.2 This column is blank if there is no primary insurance coverage OR if the primary insurance does not have a group number.
10. ICD10
10.1 The 4 columns labeled ‘ICD10’ display the first 4 diagnosis codes entered during charge posting. NOTE: Up to 12 diagnosis codes may be entered during a single posting session for each account, but only the first four are displayed on the report.
10.2 This field is mandatory for billing.
10.3 If asterisks (*) appear in these columns, electronic billing edits prevent electronic claim submission until the missing information is entered.
10.4 The Charges --► Modify screen is used to view and update all diagnosis codes associated with the charge(s).
11. Zip Code, City, and State
11.1 Displays the patient’s home address <Zip Code>, <City>, and <State> from the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen.
11.2 These fields are mandatory.
11.3 If asterisks (*) appear in any of these columns, electronic billing edits prevent electronic claim submission until the missing information is entered.
II - Column Headings on the Bottom Line: (from left to right)
The bottom line identifies billing information related to each charge line.
1. En#
1.1 Displays the encounter number for the Charges --► Encounter --► Generic (or UB Encounter, Ambulance, Physical Therapy, Chiropractic, Epogen, OB/GYN, Vision, HCAI, DME, DME Oxygen) screen associated with the charge.
1.2 This field is mandatory when posting charges on the Charges --► Charge screen, so the default is usually set to 0 (zero) to indicate that NO encounter was used.
1.3 Based on the provider’s specialty and/or the patient’s insurance, an encounter screen may or may not be needed to include additional information on paper or electronic claims. It is important to have an understanding of the billing requirements for your specialty to determine when an encounter may be needed.
1.4 The Charges --► Modify screen may be used to update the <EN#> associated with the charge.
2. Ref NPI
2.1 Displays the <NPI> field from the Utility --► Referring screen for the referring provider associated with the charge.
2.2 Asterisks (*) appear in this column when the Referring Provider’s NPI is missing or a referring provider was not entered.
2.3 This field is only required if the Ref Prov column is populated with a referring provider. See 3 below.
3. Ref Prov
3.1 Displays the referring provider’s <Referring Code> and name (<First Name> <Middle Initial> <Last Name> from the Utility --► Referring screen associated with the charge.
3.2 Asterisks (*) appear in this column when a referring provider is NOT associated with the charges.
3.3 Based on the provider’s specialty, the patient’s insurance and/or service provided, a referring provider (ordering provider or supervising provider) may or may not need to print on the CMS1500 form in box 17 or electronic equivalent.
3.4 The referring provider may be updated in the <Rdr.> field on the Charges --► Modify screen.
4. Who
4.1 Displays the responsible party (e.g., ‘P1’, ‘P2’, ‘S1’, ‘T1’, ‘G’, ‘Y’) to whom the claim is sent.
4.2 When the Billing --► Insurance --► Insurance --► Group of Patients <Primary/Sec/All (P/S/A)> field is set to ‘P All Primary Insurance’ then only charges where the ‘P1’ primary insurance or an alternate primary insurance (‘P2’, ‘P3’, ‘P4’, etc.) is the responsible party are included.
4.3 If the Pre-Billing Report is generated for ‘X-All Charges,’ then additional values may be listed:
4.3.1 ‘S1’ (or ‘S2’, ‘S3’, etc.) indicates this charge line is the responsibility of the patient’s secondary insurance and the designated secondary insurance is billed.
4.3.2 ‘T1’ (or ‘T2’, ‘T3’, etc.) indicates this charge is the responsibility of the patient’s tertiary insurance and the designated tertiary insurance is billed.
4.3.3 ‘G’ indicates that this charge line is the patient’s (or guarantor’s) responsibility and is NOT billed to insurance.
4.3.4 ‘Y’ indicates that this charge line has been ‘Put On Hold’ and is NOT billed to the patient or insurance.
4.4 The party responsible for the charge may be updated in the <Who> field on the Charges --► Modify screen.
5. Category
5.1 Displays the patient’s <Category> on the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen at the time of charge posting.
5.2 Various billing functions may be affected by the category associated with the charge, including management reports and capitation check posting.
5.3 The category code associated with the charge may be updated in the <Category*> field on the Changes --► Modify [Information] screen.
6. POS
6.1 Displays the Utility --► Facility <Facility Code> field for the place of service associated with the charge.
6.2 This field is required for billing. If this column is blank, electronic billing edits prevent electronic claim submission until the missing information is entered.
6.3 The facility where services were rendered may be updated in the <POS> field on the Charges --► Modify screen.
7. TOS
7.1 Displays the <Type of Service> field from the Utility --► Procedure --► Procedure screen for procedure code in the CPT/Mod column (see 13 below).
7.2 This informational field is NOT required for billing.
8. TxProv/FromDOS
8.1 TxProv displays the Utility --► Provider --► Provider <Provider Code> entered as the treating provider in the Charges --► Charge <Dr> field at the time of posting.
8.1.1 This field is required but only used for internal reporting purposes.
8.1.2 The treating provider may be updated in the <Dr> field on the Charges --► Modify screen.
8.2 FromDOS displays the date of service entered in the Charges --► Charge <From/Date> field at the time of posting.
8.2.1 This required field prints on the CMS 1500 form in box 24A or the electronic equivalent.
8.2.2 The <From Date> may be updated on the Charges --► Modify [Information] screen.
9. BlProv/ToDOS
9.1 BlProv displays the Utility --► Provider --► Provider <Provider Code> entered as the billing provider in the Charges --► Charge <Billing Prv> field at the time of posting.
9.1.1 This field is required for billing.
9.1.2 The <Billing Prv> may be updated on the Charges --► Modify [Information] screen.
9.2 ToDOS displays the date of service entered in the Charges --► Charge <To> field at the time of posting.
9.2.1 This required field prints on the CMS 1500 form in box 24A or the electronic equivalent.
9.2.2 The <To Date> may be updated on the Charges --► Modify [Information] screen.
10. ASI
10.1 Displays the accept assignment designation associated with the Charges --► Charge <ASI> field at the time of posting.
10.2 The <ASI> field may be updated on the Charges --► Modify screen.
11. RDX
11.1 Displays the related diagnoses pointer associated with the charge at the time of posting in the Charges --► Charge <RDX> field.
11.2 This required field prints in box 24E on the CMS 1500 form or electronic equivalent.
11.3 The related diagnosis pointer(s) may be updated in the Charges --► Modify <RDX> field.
12. Status
12.1 Displays the type of claim based on the patient’s <Category> on the Registration --► Regular --► Patient OR Registration --► Worker --► Worker screen at the time of charge posting.
12.2 The hard-coded system-assigned values include:
12.2.1 ‘A’ for a Capitated charge that is included in payment distribution of capitated checks on the Payment --► Auto Payment screen.
12.2.2 ‘C’ for a Regular charge that is NOT adjusted off at the time of posting and NOT included in the capitated payment distribution through the Auto Payment screen.
12.2.3 ‘O’ for a Company Account charge that only prints on the Company Statement and NOT on a patient statement.
12.2.4 ‘P’ for a Prepaid charge adjusted off at the time of posting.
12.3 The <Status> field may be updated on the Charges --► Modify [Information] screen.
12.3.1 Modifying the <Status> from ‘P’ to another value does NOT reverse the adjustment.
12.3.2 Changing the <Status> to ‘P’ does NOT adjust off the balance.
12.3.3 Changing the <Status> to ‘O’ does NOT put the charges on the Company Statement.
13.1 CPT displays the Utility --► Procedure --► Procedure <Code R, C, E> or <Revenue Code> as determined by the Utility --► Insurance --► Insurance <Code (R/C/E/U)> for the patient’s insurance associated with the charge AND the Charges --► Charge <Panel> field at the time of posting.
13.1.1 The procedure code cannot be modified after the charge is committed.
13.1.2 If this column is blank, electronic billing edits prevent electronic claim submission until the missing information is entered.
13.2 Mod displays the modifier attached to the procedure in the Charges --► Charge <Mod> field at the time of posting.
13.2.1 This column is blank if no modifier is associated with the charge.
13.2.2 The modifier may be updated in the Charges --► Modify <Mod> field.
14. Units
14.1 Displays the days or units entered in the Charges --► Charge <Qty> field at the time of posting.
14.2 This field should not be left blank.
14.3 The <Days Unit> field may be updated on the Charges --► Modify [Information] screen.
15. Charges
15.1 Displays the charge amount billed for each line item.
15.2 For each account, the Total line calculates the total charge amounts for all lines entered in the same posting session.
16. Credit
16.1 Displays the total of all payments and adjustments posted against each line item.
16.2 For each account, the Total line calculates the total credits for all lines entered in the same posting session.
17. Balance
17.1 Displays the remaining balance of each line item.
17.2 For each patient, the Total line calculates the remaining balance for all lines entered in the same posting session.