
Intellect™
CHARGES MENU OPTIONS
Encounter
Generic Encounter
This menu option is used to post additional claim information needed to process a patient claim.
See details on adding encounter information to a patient's account.
Video Available: Click Generic Encounter to access the link. Depending on the system set up, the media player may need to be activated. Speakers need to be attached to the workstation to hear the instructions.
Note: To view the videos, log-in through the www.primeclinical.com website. Current support is required.
Updates:
Effective version 16.05.20
In prior versions, for the Internal Control Number (ICN) to be included in the Electronic Claims, the ICN had to be entered in the <Internal Control> field. Effective this version, Intellect now pulls the ICN number from the charge. This is handled by Intellect when auto-posting is used to post payments from the payers. This modification is NOT retroactive. Additionally, this ICN now also prints on the printer EOB from Intellect.
Effective version 14.07.01
When Intellect looks for a Referring Provider (a.k.a. ordering physician), Intellect first looks at the encounter screen for either <Ordering Provider> or <Supervising Provider> and, when either is blank, Intellect looks at the Utility --►Set Up --►Parameter <Referring> setting and pulls the referring provider (a.k.a. ordering physician) based on the setting.
Effective Version 13.01.11
For clinics that submit electronic claims through WorkComp EDI:
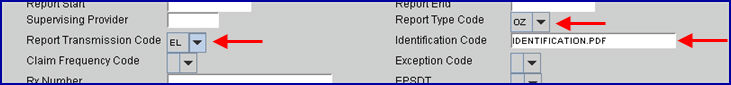
These fields should be completed on the Encounter screen to send documents electronically as a .pdf attachment to the electronic billing file:
• <Report Type Code>: Select 'OZ.'
• <Report Transmission Code>: Select 'EL.'
• <Identification Code>: Enter the unique filename of the .pdf attachment for this encounter as saved by the user under home/staff/EB_ATTACHMENT folder on the server. NOTE: PCM Users may press [F2] to view and select documents from the patient’s chart.
Example:
Please note the following in regard to Electronic Billing Attachments:
• All .pdf attachment files must be saved to the shared EB_ATTACHMENT folder on the server under the home/staff directory.
• The filename must be formatted as clinic#.acct#.uniquefilename.pdf to identify the clinic and patient account. It is strongly recommended that the date of service is used as the unique filename. For example: 1.2100.11072019.pdf
• For Intellect only clinics, the user must save the .pdf attachment file to the EB_ATTACHMENT folder on the server.
• For PCM users only, when the PCM chart document is entered using the [F2] search in the <Identification Code> field, Intellect automatically saves the file to home\staff\EB_ATTACHMENT. There is a delay between the user pressing [Add]/[Modify] and Intellect saving the file to the EB_Attachment folder, so claims should not be sent immediately.
• When a claims is sent electronically, Intellect performs a search of the EB_ATTACHMENT folder to attach the file entered in the <Identification Code> field on the Charges --►Encounter screen associated with the claim.
• If the file is not found or does not exist in the EB_ATTACHMENT folder on the server, Intellect prints 'Attachment Not found or Missing' on the Electronic Billing Report.
Effective Version 9.12.27
For clients who complete most of the Encounter screen fields with the same values for each patient, version 9.12.27 allows users to set up a 'default' record with the value to be carried over to all new Encounters.
To set up a default screen, go to Charges --►Encounter. Select the type of Encounter screen the office uses (the sample below is for Generic Encounter), then select Modify. At the <Patient Account No> field, enter 0 (zero). At the <Encounter #> field, enter 0 (zero).

Complete any field to default to all new Encounters entered.
Setting up the default encounter screen does NOT affect any encounters previously entered.
1. To add encounter information to a patient's account in Intellect, go to Charges --► Encounter --►Generic --►Add

The Add Generic screen displays:

This screen, like many in Intellect has several optional fields. The graphics in this documentation may vary slightly from actual clinics'. See the optional fields on this screen or the documentation on adding/removing fields.
2. Patients Account No 
2.1 When not already displayed, type the patient's account number.
- OR -
Type up to 6 characters of the last name and press the [F2] key. To select the code from the list, either highlight the record or press the [Enter] key, or double-click on the record.
3. Patients Name 
3.1 The patient's name displays. This is a read-only field and may not be modified.
3.2 The display is formatted Last, First.
4.1 This number is assigned automatically when adding a new record.
4.2 This number is used to individually display and identify this encounter.
5.1 Type a meaningful description for this encounter.
5.2 Effective version 18.04.11, for users who would like to include the Date of Admission (DOA) and Date of Discharge (DOD) on any hospital charges coming from their HL7 Vendor, Intellect inserts that information into a Generic Encounter which populates this <Encounter Description> field with the words IMPORTED DATA, populates the <Hospitalization From> field on this screen with the Date of Admission listed in the PV1-44, populates the <Hospitalization To> field on this screen with the Date of Discharge listed in the PV1-45, and attaches the Encounter number to the charge data being imported. NOTE: To facilitate this option, the <Attach Encounter> field on the Utility --►Set Up --►Parameter must not be set to ‘N’ or ‘X’.
6.1 Type the date of injury for a Workers’ Comp case.
6.2 Effective version 14.09.29: This field is no longer required if the <DOI> field on the Registration --►Worker --►Worker Insurance screen is completed since Intellect pulls the date from that field to complete the CMS 1500 or electronic equivalent.
6.3 Effective version 13.12.12: For Workers’ Comp patients only (Utility --►Category <Type> = ‘W’ or ‘F’), Intellect completes Box 14 on the CMS form with the date and qualifier 439.

Or, when used for electronic claims submission, this date goes in Loop 2400 DTP*439*.
7.1 Type the date for claims that include an order (order for service or supplies to be billed and/or reported).
7.2 For electronic claims submission, this goes in Loop 2300 DTP*180.
8.1 Effective version 13.12.12: Information is pulled from this field to fill-in Box 15 on the CMS 1500 with qualifier 455.
8.2 Type the date of 'Last X-ray' for spinal manipulation. For electronic claims submission, this date goes in Loop 2400 DTP*455.
9.1 Type the authorization number for the treatment given by the insurer for this treatment.
9.2 Intellect completes Box 23 on the CMS 1500 form with this number.

Or, when used for electronic claims submission, this number goes in Loop 2300 REF*G*1.
10.1 Type the date the patient was last seen by the attending physician for the qualifying condition related to the services performed.
10.2 This is a required field when services involve an independent PT, an occupational therapist, or physician involving routine foot care.
10.3 Intellect completes Box 14 on the CMS 1500 form with the date and qualifier 304.
Or, when used for electronic claim submission, this date goes in Loop 2300 DTP*304*D8*.
11.1 This is an informational field. Enter the <Total Authorized Visits> (see below) minus the number of visits that have taken place.
11.2 This value is displayed in the Charges --►Charge <Visit No> field.
12.1 This is an informational field. Enter the total visits as authorized by the insurer.
13.1 If the default 'null/blank' option is selected for this field, the program pulls the Charges --►Encounter <Delay Reason Code> field and, for paper claims, prints it in Box 24C on the CMS 1500 Claim form. BUT, if billing electronically, the <Delay Reason Code> is not billed when the Encounter <Emergency (Y/N)> is null. Instead, this goes in 837 Electronic Claims Submission Equivalent Loop 2400 SV109.
NOTE: On the CMS 1500 Claim form, for all insurance types in Utility --►Insurance <Insurance Type>, Box 24C prints from the patient's Charges --►Encounter screen when the <Encounter #> field is associated with the charges being printed (Charges --►Charge OR Charges --► Modify <EN#> field) unless the Charges --►Encounter <Emergency (Y/N)> field is null.
13.2 Select 'Y' (yes) for an emergency to place a 'Y' in Box 24C of the CMS 1500 form. See sample below.
13.3 Select 'N' for a non-emergency. Nothing prints in Box 24C.
14.1 Type the beginning effective date authorized by the insurer for this treatment.
15. Authorization To 
15.1 Type the effective end date authorized for this treatment.
15.2 When posting charges linked to this encounter (in Charges --►Charge) and the date of service is not within this date range, this warning displays:

Click [Yes] to continue.
16.1 Type the admit date of the patient, if hospitalized.
16.2 Intellect completes Box 18 of the CMS 1500 form with this date:
Or, when used for electronic claims submission, this date goes in Loop 2300 DTP*435.
16.3 Effective version 18.04.11, for users who would like to include the Date of Admission (DOA) and Date of Discharge (DOD) on any hospital charges coming from their HL7 Vendor, Intellect inserts that information into a Generic Encounter which populates this <Hospitalization From> field with the Date of Admission listed in the PV1-44, populates the <Hospitalization To> field (see below) with the Date of Discharge listed in the PV1-45, populates the <Encounter Description> field on this screen with the words IMPORTED DATA, and attaches the Encounter number to the charge data being imported. NOTE: To facilitate this option, the <Attach Encounter> field on the Utility --►Set Up --►Parameter must not be set to ‘N’ or ‘X’.
17.1 Type the discharge date of the patient, if hospitalized.
17.2 Intellect completes Box 18 of the CMS 1500 form with this date:
Or, when used for electronic claims submission, this date goes in Loop 2300 DTP*096.
17.3 Effective version 18.04.11, for users who would like to include the Date of Admission (DOA) and Date of Discharge (DOD) on any hospital charges coming from their HL7 Vendor, Intellect inserts that information into a Generic Encounter which populates this <Hospitalization To> field with the Date of Discharge listed in the PV1-45, populates the <Hospitalization From> field (see above) with the Date of Admission listed in the PV1-44, populates the <Encounter Description> field on this screen with the words IMPORTED DATA, and attaches the Encounter number to the charge data being imported. NOTE: To facilitate this option, the <Attach Encounter> field on the Utility --►Set Up --►Parameter must not be set to ‘N’ or ‘X’.
18. Place of Service 
18.1 This is an informational field and does not print.
18.2 Type the Utility --►Facility <Facility Code>, or type up to 6 characters of the description and press the [F2] key. To select the code from the list, either highlight the record, press the [Enter] key, or double-click on the record. Alternately, after clearing the field, press the [F2] key twice to view the entire list of codes.
19.1 This field is used only for lab work done outside the office that will be billed to the patient's insurance and the lab bills the clinic.
19.2 Enter the facility code for the lab, or press [F2] to access the Searching Facility screen from which to search for the <Facility Code> on the Utility --►Facility screen.
19.3 If Utility --►Procedure --►Procedure <Status> = 'L', and a Facility Code is entered in this field, then Intellect prints an ‘X’ in the Yes box for Box 20 OUTSIDE LAB on the CMS 1500 form.
![]()
Or, when used for Electronic claims submission, the Utility --►Facility information appears in Loop 2310C NM1*QB*2*****.
20.1 Use this area to write an appropriate description.
20.2 The description appears in Box 19 of the CMS 1500 form:

Or, when used for electronic claims submission, this text goes in Loop 2300 NTE*ADD*.
20.3 Since it is required to add notes, effective version 9.12.28 (February 2012), Intellect pulls the comments entered into this field and enters them into Box 19 of the Worker CMS 1500.
Note: This change for the CMS 1500 form is not automatically added with the update. To have this changed, call Prime Clinical Systems and request the form be updated.
20.4 Effective version 16.05.20: The field size was increased to accommodate the new CMS requirement in which the dates of service for at least 13 antepartum visits are entered for Global Billing of OB care and delivery, whether sent on paper or electronically.

21.1 This field allows users to type a date instead of a description for Box 19 on the CMS 1500 form.
21.2 If a user types both a date and description, the description is appended.
22.1 Type the date of the first symptom.
22.2 Effective version 13.12.12: Information is pulled from this field to fill-in Box 14 on the CMS 1500 form with qualifier 431.
Intellect completes Box 14 on the CMS 1500 with this date.

Or, when used for electronic claims submission, it is added to Loop 2400 DTP*431*D8*.
22.3 Note: This date does not apply to Worker’s Comp Utility --►Category <Type> 'W' or 'F'.
23.1 Type the date of the first consultation.
23.2 If patient's insurer is NOT Medicare, Medi-Medi, or Medi-Cal (Medicaid ), then Intellect completes Box 15 with this date.

23.3 Effective version 13.12.12: For Property & Casualty, information is pulled from this field to fill-in Box 15 on the CMS 1500 form with qualifier 444.
24. Ordering Provider 
24.1 Type the code for the Ordering Provider, if required for a service or if a supply is ordered by a provider that is different from the rendering provider for this claim.
24.2 This code pulls information from Utility --►Referring <Referring Code>.
24.3 Effective version 13.10.29: For the CMS 1500 form, Intellect completes the Ordering Provider’s name in Box 17 with qualifier DK (for Ordering Provider) and the provider’s NPI in Box 17b.

Or, when used for electronic claim submission, Loop 2310E NM1*DK.
25. Similar Symptom Date 
25.1 If the patient has had a similar symptom, type the date in this field.
25.2 This is used for electronic claims submission Loop 2400 DTP*438*D8*.
26.1 Select 'F' for full time, 'P' for part time, or 'N' for unemployed.
26.2 This is not used for electronic submission.
27.1 Select 'F' for full time, 'P' for part time, or 'N' for not enrolled as a student.
27.2 Electronic claims submission fills Loop 2300 CLM11 - 1 through CLM11.
28.1 Indicate whether or not this treatment is related to an accident.
28.2 Select the default 'N' if it is not related to an accident.
28.3 Select 'A' for an automobile accident. Selecting 'A' places an 'X' on the CMS 1500 form in Box 10b Yes (see screen save below), and also places the resident state code in the <Place> field.
28.4 Select 'O' for another type of accident. Selecting 'O' places an 'X'on the CMS 1500 form in Box 10c Yes:

Electronic claims submission Loop 2300 CLM11 - 1 through CLM11 - 3:
AA Auto Accident
AB Abuse
AP Another Party Responsible
EM Employment
OA Other Accident
Note: When rebilling claims to indicate corrected claims or replacement claims with internal control numbers, this field may not be left blank -- a selection must be made. In addition, make sure to enter the proper <Claim Frequency Code> and <Internal Control> numbers on this screen.
29.1 Effective version 14.09.29: If the <Employment> field on the Registration --►Worker --►Worker Insurance screen is set to 'Y', Intellect sets this field to 'Y.'
29.2 Offices with a version prior to 14.09.29 should select 'Y' or 'N' to indicate whether or not the condition is related to employment.
29.3 Intellect places an 'X' in Box 10a on the CMS 1500 form.
Electronic claims submission Loop 2300 CLM11 - 1 through CLM11 - 3:
AA Auto Accident
AB Abuse
AP Another Party Responsible
EM Employment
OA Other Accident
30.1 Effective version 9.12.1 New drop-down list.
30.2 Medicare status codes are required for Charpentier claims (in all other circumstances, these codes are optional).
30.3 This is used for Medi-Cal patients who fall into the category of Alien Residents of Medicare Eligibility Age, but do not have Medicare coverage (consult Medi-Cal billing).
30.4 To view the list of codes with descriptions, place the pointer in the <Medicare Status> field and press the [F2] key. To view the list of only the codes, either click on the arrow OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
30.5 If Utility --►Insurance --►Insurance <Insurance Type> = 'D' or 'I,' Intellect completes Box 22 on the CMS1500 form with this code.
Note: For all options except '0', documentation is required. Refer to the Medicare/Medi-Cal Crossover Claims: CMS-1500 Section in the appropriate Part 2 Manual for additional information.
31.1 Type the first date the patient is unable to work due to this condition. This is required on claims where this information is necessary for adjudication of the claim (e.g., workers compensation claims involving absence from work).
31.2 Intellect completes Box 16 on the CMS 1500 form.
31.3 This is used in electronic claims processing Loop 2300 DTP*297.
32. Able to Return to Work 
32.1 Type the date the patient is able to go back to work.
32.2 Intellect completes Box 16 on the CMS 1500 form.
Or, when used for electronic claims submission, it is added to Loop 2300 DTP*296*D8*.
33.1 Type the date the disability began.
33.2 This replaces <Unable To Work From> on the CMS 1500 form for students, unemployed, or persons unable to do their current job.
33.3 This is used in electronic claims processing Loop 2300 DTP*360*D8.
33.4 This does not display on the CMS 1500 form.
34.1 Type the date able to return to full work, if applicable.
34.2 This replaces <Unable To Work From> on the CMS 1500 form for students, unemployed, or persons unable to do their current job.
34.3 This is used in electronic claims processing Loop 2300 DTP*361*D8.
34.4 This does not display on the CMS 1500 form.
35.1 This is an informational field for Medi-Cal patients only.
35.2 Type the Medi-Cal Share of Cost Code for this patient. View the list of AID Codes.
36.1 If Medi-Cal is primary (Utility --► Insurance --► Insurance <Insurance Type> = D), Intellect completes Box 10 d on the CMS 1500 form with this amount.
36.2 Type the Medi-Cal portion of cost for patient.
NOTE: Do not enter decimal points or dollar signs. Enter full dollar and cents amounts, even if the amount is even. For example $4.00 is entered as 400.
37.1 To view the list of codes with descriptions, place the pointer in the <Family Planning> field and press the [F2] key. To view the list of only the codes either click on the arrow OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
37.2 For MCAL patients (Utility --►Insurance --►Insurance <Insurance Type> = D), Intellect completes box 24H on the CMS 1500 form.
![]()
38.1 This is for electronic claims submission Loop 2300 CLM 20. This element may be used if a particular claim is being transmitted in response to a request for information (e.g., a 277), and the response has been delayed. This is required when a claim is submitted late (past contracted date of filing limitations) and any of the codes below apply.
38.2 For paper claims, this prints on the 1500 Claim Form if the <Emergency (Y/N)> field on this screen is 'null/blank' (as opposed to Yes or No). BUT, if billing electronically, the <Delay Reason Code> is not billed when the Encounter <Emergency (Y/N)> is null. The <Delay Reason Code> transmits in electronic claims submission Loop 2300 CLM 20.
38.3 To view the list of codes with descriptions, place the pointer in the <Delay Reason Code> field and press the [F2] key. To view the list of only the codes, click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.

39.1 If therapy is involved, type the date the therapist was last certified.
39.2 This is used in electronic billing.
40.1 This is required on Medicare electronic claims to indicate 'assumed care date' and for situations where providers share postoperative care (global surgery claims). It fills Loop 2300 DTP*090*D8.
40.2 Assumed Care Date is the date care was assumed by another provider during post-operative care.
40.3 Effective version 13.12.12: Information is pulled from this field to fill-in Box 15 on the CMS 1500 form with qualifier 090.
41.1 Required on Medicare claims to indicate 'relinquished care date' for situations where providers share postoperative care (global surgery claims). It fills Loop 2300 DTP*091*D8.
41.2 Relinquished Care Date is the date the provider filing this claim ceased post-operative care.
Example: Surgeon 'A' relinquished post-operative care to Physician 'B' five days after surgery. When Surgeon 'A' submits a claim/encounter 'A', Intellect uses code '091 - Report End' to indicate the day the surgeon relinquished care of this patient to Physician 'B'. When Physician 'B' submits a claim/encounter 'B', Intellect uses code 090 - Report Start patient from Surgeon 'A.'
![]()
41.3 Effective version 13.12.12: Information is pulled from this field to fill-in Box 15 on the CMS 1500 form with qualifier 091.
42. Supervising Provider 
42.1 Type the code for the Supervising Provider when required
42.2 This code pulls information from Utility --►Referring <Referring Code>.
42.3 Effective version 13.10.29, For the CMS 1500 form, Intellect completes the Supervising Provider’s name in Box 17 with qualifier DQ (for Supervising Provider) and the provider’s NPI in Box 17b.

Or, when used for electronic claims submission, Loop 2310D NM1*DQ.
43.1 This field is used to designate a supplemental report type that is forwarded separately. It works with the <Report Transmission Code> and <Identification Code> fields on this screen. When sending attachments with the electronic claim files, all three fields are required.
43.2 If the <Report Type code>, <Report Transmission Code>, and <Identification Code> fields are completed on this screen, the entered values print in the third part of Box 81 of the UB04 form. If they are not completed, the third part of Box 81 is blank.
Note: The changes to UB04 forms is not automatically added with the 9.12.29 update. To have these changes, call Prime Clinical Systems and request the form be updated.
43.3 To view the list of codes with descriptions, place the pointer in the <Report Type Code> field and press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.

43.4 WorkComp EDI users: Select option 'OZ' if sending an attachment with the electronic claim file.
44.1 This field is used to designate the method of transmission when supplemental claim information is required with electronic billing.
44.2 This field works with the <Report Type Code> and <Identification Code> fields on this screen. When sending attachments with the electronic claim files, all three fields are required.
44.3 If the <Report Type Code>, <Report Transmission Code>, and <Identification Code> fields are completed on this screen, the entered values print in the third part of Box 81 of the UB04 form. If they are not completed, the third part of Box 81 is blank.
Note; The changes to UB04 forms are not automatically added with the 9.12.29 update. To have these changes, call Prime Clinical Systems and request the form be updated.
44.4 To view the list of codes with descriptions, place the pointer in the <Report Transmission Code> field and press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
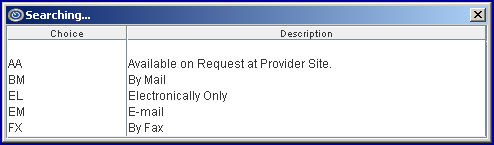
44.5 WorkComp EDI users: Select option 'EL' if sending an attachment with the electronic claim file.
45.1 This is used for electronic billing when attaching supplemental claim information.
45.2 This field works with the <Report Type Code> and <Report Transmission Code> fields on this screen. When sending attachments with the electronic claim files, all three fields are required.
45.3 If the <Report Type Code>, <Report Transmission Code>, and <Identification Code> fields are completed on this screen, the values entered print in the third part of Box 81 of the UB04 form. If they are not completed, the third part of Box 81 is blank.
Note: The changes to UB04 forms are not automatically added with the 9.12.29 update. To have these changes, call Prime Clinical Systems and request the form be updated.
45.4 Type the Attachment Control Number from the pre-printed MEDI-CAL CLAIM Attachment Control Form. The form must accompany the supporting documentation.
Note: When completing the encounter record, it is recommended to include the ATTACHMENT CONTROL NUMBER as part of the Encounter Description.
45.5 WorkComp EDI users, please note: Enter the name of the .pdf attachment file if sending the attachment with the electronic claim file. Note: Effective version 13.12.12, Intellect began including a K3 packet with the claims sent to WorkComp EDI as part of the attachments.
45.5.1 For clients using PCM. Effective version 14.11.10, use the <PCM Import> field on the Utility --►Insurance --►Tele Com screen to indicate whether or not the K3 packet files, in .pdf format, should be imported to PCM.
45.5.2 All .pdf attachment files must be saved to the shared EB_ATTACHMENT folder on the server under the home\staff directory. NOTE: The name of the .pdf file is formatted as clinic#.account#.uniquefilename, but only the unique filename portion is entered in this field. For example: Type 2177 for file saved as 1.1007.2177.
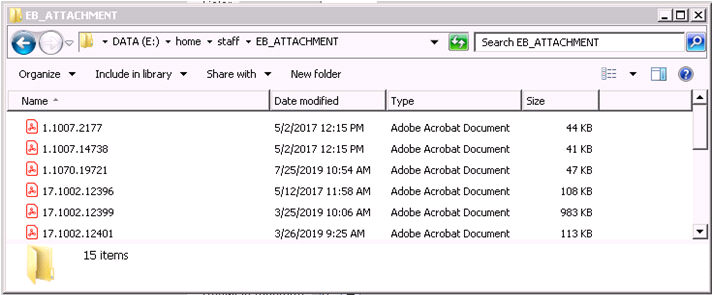
45.5.2.1 For clients using Intellect only: When user generated files are saved to the EB_ATTACHMENT folder, it is strongly recommended that the name contains the date of service.

45.5.2.2 For clients using PCM. When documents are automatically imported from the PCM chart, the Document ID is used as the unique filename, see 45.5.3 below.
45.5.3 For clients using PCM. Effective version 14.07.01: Users are able to select documents from the PCM chart to send as .pdf attachments.
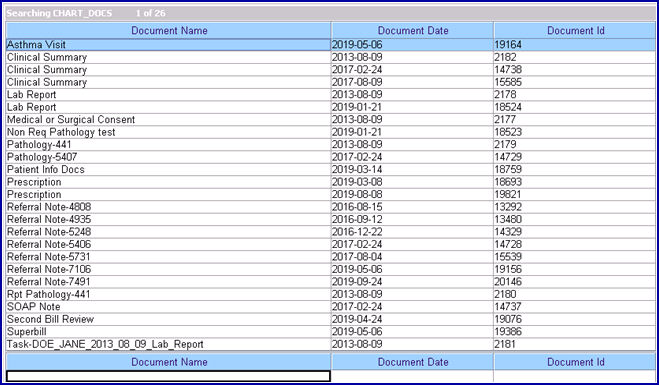
45.5.3.1 With the focus in this field, press the [F2] key twice to display a list of document files pulled from the patient’s chart in PCM.
NOTE: The list does NOT include files generated in Intellect or manually saved to the /home/staff/EB_ATTACHMENT folder.
45.5.3.2 To display only a certain type of file, enter the beginning letters of the file and then press [F2].
45.5.3.3 Click on the appropriate file to select it. Multiple files may be selected by holding down the [Ctrl] and [Shift] keys while clicking on the desired files. The file's Document Id displays.
45.5.3.4 NOTE: There is a delay between the user pressing [Add]/[Modify] and Intellect saving the file to the EB_Attachment folder, so claims should not be sent immediately.
46.1 The Claim Frequency Code is used only for electronic billing Loop 2300 CLM05-3, and indicates what type of claim it is. For example, an original submission, corrected claim which is being resubmitted, a replacement claim, or a voided claim. The default is set to 1 Original Submission. Prior to adding this field on the Encounter screen, the system submitted all claims with Claim Frequency Code '1'.
46.2 To view the list of codes with descriptions, place the pointer in the <Claim Frequency Code> field and press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
Note: The Internal Control Number and the Frequency Code may be included on the paper claim if this field and the <Internal Control Number> field (see below) are completed.
46.3 Box 22a & b on Worker CMS 1500 forms are for replacement claims, corrected claims, or appealed claims. In other words, when a claim has been rejected and needs to be resubmitted. Effective version 9.12.28 (February 2012), Section (a) of this box is filled with a 7 or 8, as entered into this field. Section (b) of this box is filled with the Attachment Control Number from the pre-printed MEDI-CAL CLAIM Attachment Control Form, as entered in the <Identification Code> field on this screen.
Note1: This change for the CMS 1500 form is not automatically added with the update. To have this change, call Prime Clinical Systems and request the form be updated.
Note2: The form must accompany the supporting documentation.
46.4 When rebilling claims to indicate corrected claims or replacement claims with internal control numbers, make sure to enter the proper code in this field. Additionally, the proper code should be entered in the <Internal Control> field on this screen and the <Related Accident> field on this screen may not be left blank.
46.5 When making an appeal for a Worker's Comp claim, in addition to this field, the <Internal Control>, <Appeal Type>, and <Appeal Documentation File> fields MUST be filled.
46.6 Effective version 18.08.31: When this field is set greater than 1 and the <Internal Control> field is blank, the ICN # that comes with the ERA file is printed in Box 22 on the HCFA 1500 and also sent electronically.
47.1 This is required for electronic billing when providers are required by state law (e.g., New York State Medicaid) to obtain authorization for specific services, but, for the reasons listed in REF02, performed the service without obtaining the service authorization. Check with your state Medicaid to see if this applies in your state.
47.2 To view the list of codes with descriptions, place the pointer in the <Exception Code> field and press the [F2] key. To view the list of only the codes either click on the arrow, OR press the → (right arrow) on the keyboard. To select, double-click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.

48.1 Enter the unique identification number assigned by the pharmacy or supplier to the prescription. It fills Loop 2410 REF02 with the Qualifier XZ.
49.1 This number is included in the electronic transmission for all claims. It is a number assigned by the payer to identify a claim. The number is usually referred to as an Internal Control Number (ICN), Claim Control Number (CCN), or a Document Control Number (DCN). CLM, 2300 REF02 is the Loop and segment:
CLM*1.608.1.491.G*250***11:B:7*Y*A*Y*Y*P
REF*F8*20024E011000 ß
49.2 The Internal Control Number and the Frequency Code may be included on the paper claim if this field and the <Claim Frequency Code> field (see above) are completed on the encounter.
49.3 When claims are corrected claims or replacement claims with internal control numbers, make sure to enter the proper code in this field. Additionally, the proper code should be entered in the <Claim Frequency Code> field, and the <Related Accident> field may not be left blank.
49.4 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Appeal Type>, and <Appeal Documentation File> fields on this screen MUST be filled.
49.5 In versions prior to 16.05.20, for the ICN to be included in the Electronic Claims, the ICN had to be entered in this <Internal Control> field. Effective version 16.05.20, Intellect now pulls the ICN number from the charge. This is handled by Intellect when Autoposting is used to post payments from the payers. This modification is NOT retroactive. Additionally, this ICN now also prints on the printer EOB from Intellect.
49.6 Effective version 18.08.31: When this field is blank and the <Claim Frequency Code> field is set greater than 1, the ICN # that comes with the ERA file is printed in Box 22 on the HCFA 1500 and also sent electronically.
50.1 This field is used to identify the level of the appeal, if needed.
50.2 Use the drop-down list and select the appropriate option:
50.3 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Internal Control>, and <Appeal Documentation File> fields on this screen MUST be filled.
51.1 If there is documentation that needs to be sent to the insurance company, enter the file name of the documentation.
51.2 Files with valid file names are sent directly to the insurance company.
51.3 Effective version 14.07.01:
Clients with Intellect only:
51.3.1 Create and save Appeal Document(s) files in the /home/staff/EB_ATTACHMENT folder. SBRs may also be saved as a .pdf to the /home/staff/EB_ATTACHMENT folder and attached as appeal documents.
51.3.2 Type the exact file name in this field. Note: This field is case-sensitive.
Clients with both Intellect and Patient Chart Manager (PCM) only:
51.3.3 With the focus in this field, press the [F2] key twice to display a list of document files pulled from the Progress Notes in PCM (the list does NOT include files generated in Intellect or manually saved to the /home/staff/EB_ATTACHMENT folder).
51.3.4 To display only a certain type of file, enter the beginning letters of the file and then press [F2].
51.3.5 Click on the appropriate file to select it. Multiple files may be selected by holding down the [Ctrl] and [Shift] keys while clicking on the desired files. The file's Document Id displays.
51.4 When making an appeal for a Worker's Comp claim, in addition to this field, the <Claim Frequency Code>, <Internal Control>, and <Appeal Type> fields on this screen MUST be filled.
52.1 Effective version 14.02.04.
52.2 This field was added for use with clinical trials for medicines, procedures, etc.
52.3 Enter the 8-digit clinical trial registry number (CTN).
52.3.1 For CMS 1500 forms: When the <Project Identified> field is populated with the 8-digit CTN, Intellect prints it in Box 19, preceded by 'CT'. Do not enter 'CT' as part of the number when entering it in this field.
52.3.2 For 837 Professional Claims: When the <Project Identified> field is populated with the 8-digit CTN, Intellect includes P4 in the Loop 2300, REF02, REF01. For example, REF*P4*12345678.
53. When the information is completely entered, select one of these options:

53.1 Click [Add] to clear the screen and return the focus to the <Patients Account No> field, saving the new encounter.
53.2 Click [Clear] to display this message:

53.2.1 Click [Yes] to clear the screen and return the focus to the <Patient Account No> field, saving the new encounter.
53.2.2 Click [No] to clear the screen and return the focus to the <Patient Account No> field without saving.
53.3 Click [Exit] to display this message:
53.3.1 Click [Yes] to clear the screen and return the focus to the main Intellect screen saving the new encounter.
53.3.2 Click [No] to clear the screen and return the focus to the main Intellect screen without saving.
Related Topics: 837 Health Care Claim Review or CMS 1500 Claim Form Review
Offices who do not have these fields on their screen and would like to have them should contact PCS support to add them.
1.1 Type the date of the first observable conditions.
1.2 Effective version 13.12.12: Information is pulled from this field to complete Box 15 on the CMS 1500 form with the date and qualifier 453.

1.3 For electronic claims submission, this date is required when Loop 2300 CR2018 = ‘A’ or ‘M’, the claim involves spinal manipulation and the payer is Medicare. This date is found in Loop 2400*DTP*453.
2. Discharge Date ![]()
2.1 Type the date the patient was released from doctor’s care for related treatment.
2.2 This is for information only and does not print.
3.1 This field is used for Medicaid Illinois Form HFS 2360.
3.2 If a provider completed a Healthy Kids screening, or if diagnostic and treatment services were provided because of a Healthy Kids screening, select 'Y' (yes).
3.3 Intellect places an 'X' in the appropriate Box 23A Illinois DPA 2360.
![]()
4.1 Type the date of the initial treatment for spinal manipulation. This is required for Chiropractic claims.
4.2 Effective version 13.12.12: Information is pulled from this field to complete Box 14 on the CMS 1500 with the date and qualifier 431.
![]()
4.3 For electronic claims submission, this date goes in Loop 2400*DPT*454.
5.1 This field is used for Illinois DPA 2360.
5.2 It is used to bill for payment for a Sterilization or Abortion provider.
5.3 Intellect places an 'X' in the appropriate Box 23c DPA 2360.
