

Intellect™
PAYMENT MENU OPTIONS

Auto Payment
Post Payments and Adjustments
This menu option is used to post payments and adjustments automatically to patient accounts. When certain configuration requirements have been met, either ERA or regular check payment/adjustment posting for Medicare, Medi-Cal, and/or Capitated (Pre-Paid) contracts can be accomplished. This process may also be set for automation.
Video Available: Click Payment Auto Payment ERA to access the link. Depending on the system set up, the media player may need to be activated. Speakers need to be attached to the workstation to hear the instructions.
Note: To view the videos, log-in through the www.primeclinical.com website. Current support is required.
See details on using the Auto Payments feature in Intellect to post an Electronic Remittance Advice (ERA).
Updates:
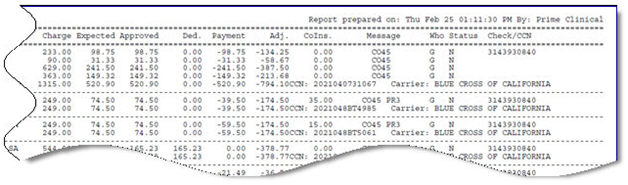
Effective version 21.02.26, Intellect now includes the Insurance Code attached to the charges in the ERA Report. The information prints below the Check/CCN #, as shown below:
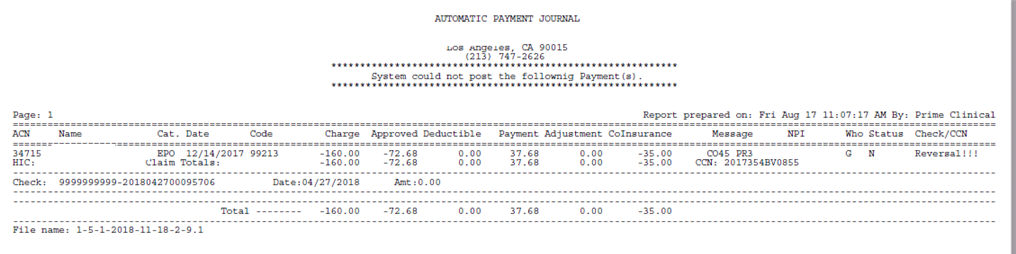
Effective version 18.08.31: In previous versions, when a payer was taking back payment and/or adjustments to previously paid and adjusted charges, the program printed the information about the deduction, including the working Reversal on the ERA, and it was required to manually do the work to adjust the charge(s):
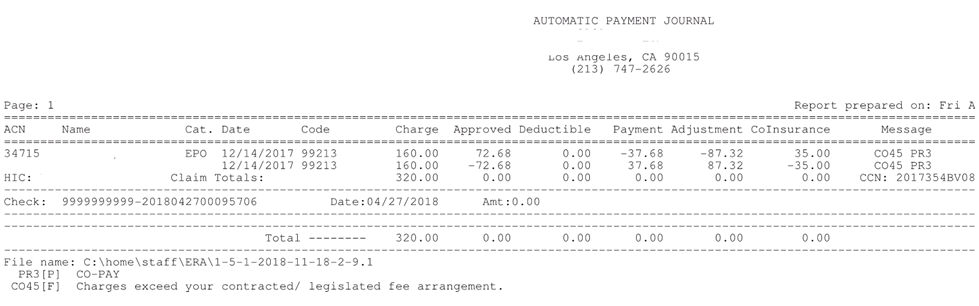
As of this release, Intellect makes the reversal of the payments and adjustments from the ERA file:
When an Electronic ERA is used to post payments, an Internal Control Number (aka ICN) is always included in the file. Effective Intellect version 16.05.20, the ICN number is now included in the Electronic claim file when billing the secondary.
Effective version 13.08.20 - If your office is receiving ERAs direct to/from Medicare, your ERA files no longer print. See <File Name> 6.3 and 19.1.1 Printer Properties for additional information.
Effective version 9.12.14 - Modification:
If an office uses the same submitter number for multiple clinics, the payments for all clinics are in the same ERA file. Prior to the version 9.12.14 update, when posting ERA files via Payment --►Auto Payment, the payments for any clinic other than the one in which the clinic was posting would print on the 'Error Report'.
Effective this update, the 837 CLM segment prefixes the account number with the clinic designation. With this change, Intellect reads the clinic designation from the CLM segment and, therefore, no longer prints payments for other clinics on the Error Report.
The automated ERA task continues to run in only one clinic using the same submitter number. However, the Error Report now only prints the records for only the clinic in which it is run. Therefore, it is important to remember to run Payment --►Auto Payment in each clinic which shares the same Submitter Number.
Note: This affects only the ERA files received for claims which are billed after receiving this update.
Electronic Remittance Advice (ERA): Posting via Auto Payment
Note: Prior to using this option, the appropriate account must be established with the paying agency or clearinghouse. This information is then entered into the Utility --►Insurance --►Tele Com screen.
There is essentially a two-step process with the ERA. First, pick up the ERA file from the transmitting site. Second, post the file to automatically credit the patient accounts. Ultimately, these can be combined into one step, if so desired.
1. To use the Auto Payments feature in Intellect, go to Payment --► Auto Payment
The Auto Payment screen displays:
2.1 Accept the default OR use the drop-down list to make an alternate selection.
2.2 Press the [F2] search key to display the valid choices:
Effective version 16.10.11:
As of version 16.10.11, the <Carrier Type> associated with the Utility --►Insurance --►Insurance <Electronic Billing> field carrier types are no longer required for use in the Payment --►Auto Payment screen. All carrier types outside of C, P, A, B, and W now use ‘Insurance.’ To accommodate this change, the drop-down list was changed. Please note:
Insurance replaces options M, I, and X. For Utility --►Insurance --►Insurance <Electronic Billing> field carrier types outside of the values shown above, select Insurance.
Pre-Paid Charge replaces option 'C.'
Pre-Paid Balance replaces option 'P.'
Pre-Paid Approved replaces option 'A.'
Pre-Paid Percent replaces option 'B.'
Write off charges replaces option 'W.'
All versions prior to 16.10.11:
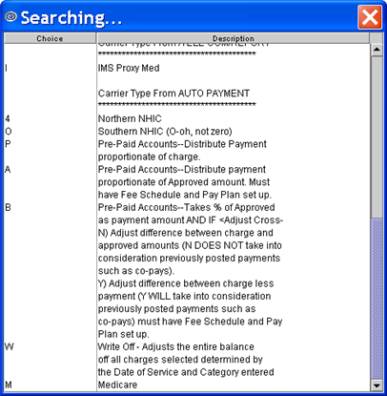
Note: Option 'O' is the capital letter O, NOT zero).
3. From 
3.1 Leave blank for this option (used for Capitated accounts).
4. To 
4.1 Leave blank for this option (used for Capitated accounts).
5. Payment 
5.1 Leave blank for this option (used for Capitated accounts).
6. File Name 
6.1 Enter the 'File Name' noted on the ERA file printout (see file samples below).
6.2 Effective Version 9.12.27: After completing the <Carrier Type> when posting an ERA/ERN file from the Auto Payment screen, rather than typing in the file name, it can now be searched for by pressing [F2] in the <File Name> field. Press the [F2] key to list the ERA/ERN files in the clinics ERA directory. The files are listed in order by the file name. The first value in the <File Name> is the clinic in which the ERA/ERN file was picked up. If your office bills from multiple clinics, the files are listed in the clinic order of the clinic from which the ERA/ERN is picked up.
Click on a file name to display it in the <File Name> field. In the samples below, the first file on the above list was clicked on and, therefore, displays in the <File Name> field:
6.3 Effective version 13.08.20 - If your office is receiving ERAs direct to/from Medicare, your ERA files no longer print. To print or view the ERA files that have been downloaded, the <Receiver>, <Payer identifier>, and <Payor & Office Code> fields on the Utility --►Insurance --►Insurance screen, and the <ISA Receiver ID (08)> and <GS Receiver ID (03)> fields on the Utility --►Insurance --►Tele Com screen must be set up as indicated in those options.
Medicare Electronic 999, 277 and ERA Reports (August 20, 2013)
Due to the current nature of the set up in Intellect for the downloading of the files from your Medicare mailbox using Ability, the ERA files are being downloaded during the same session as the 999 and 277 reports and WILL NOT PRINT.
Your office is required to check the ERA folder for any NEW ERAs that have been downloaded, and manually print the Report from the AutoPosting screen.
See 19.1.1 Printer Properties for printer information.
7. Insurance Code 
7.1 Enter the Utility --►Insurance --►Insurance < Insurance Co. Code>.
8.1 Leave blank for this option.
9.1 Leave blank for this option.
10.1 Select 'Pay & Report.'
11. Check 
11.1 Leave blank when posting all check numbers, payments, and adjustments.
11.2 When posting individual check numbers, payments, and adjustments ONLY, type the specified check number.
12.1 This is used for certain ERA.
12.2 Accept the default OR use the drop-down list to make an alternate selection.
The default is set to 'No - Do NOT print the secondary Ins CSM 1500 form' (formerly option 'N').
12.3 For a description of each option, press the [F2] search key. Double-click on an option to select it.
Effective version 16.10.11:
Effective version 17.02.17, when selecting either the 'HCFA and EOMB for all charges' or 'HCFA and EOMB for charges not crossed over' and an ERA/835 contains Dates of Service (DOS) that are the same and have a different visit number, the program prints a separate HCFA and EOMB. If however, an ERA/835 has multiple DOS and the visit number (CLP) is the same, Intellect does not separate the charges that print on the HCFA and EOMB.
Versions prior to 16.10.11:
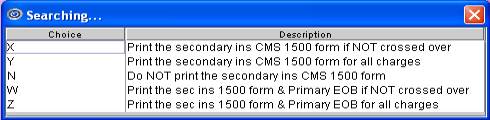
Note: Effective version 15.09.02, for options W and Z, the Check No and Payment Date fields may be added if it is desired to have this data on Report Designer. Please contact PCS Support for additional information.
13. Provider Code 
13.1 Leave blank for this option (used for Capitated accounts).
14. Category Code 
14.1 Leave blank for this option (used for Capitated accounts).
15. Batch No 
15.1 Prime Clinical Systems recommends the assignment of a Batch No when using the bulk payment methods. If a posting error occurs; i.e., posting the wrong amount, the same check twice, etc., if a Batch No was entered when applying the payment and adjustment transactions, then they may be reversed/removed using Utility --►Maintenance --►Reverse Entry , provided the clinic date has not been changed
15.2 This is used as a future reference to look up payments.
15.3 Version 9.12.14 - Modification. This field has been increased to 20-characters to match the allowed number of characters in both the Payment --►Open Item and Charges --►Charge screen.
16.1 This field controls whether or not the co-insurance and/or deductible amounts are adjusted off for Medi-Medi crossover claims where the Utility- -►Insurance --► Insurance <Insurance Type> = 1 (Medicare/Medicaid) for the patient’s primary insurance.
16.1.1 'No' does not adjust off the balance.
16.1.2 ' Yes' adjusts off the balances. NOTE: The amounts listed in the ‘CoInsurance’ and ‘Deductible’ columns on the Automatic Payment Journal are adjusted off for Medi-Medi crossover claims.
16.1.3 Effective version 17.02.17 ‘Exclude Deductible’ allows the automatic write off for Medi-Medi crossover claims without writing off any amounts that are patient responsibility.
17. Credit Card Payment 
17.1 Effective version 14.03.20, this field was added to the Payment --►Auto Payment screen. This is a Y/N field and works the same as the ☐ Credit Card Payment option on the Payment screen.
17.2 The Autopayment feature posts all open balances for line item charges with payments in the ERA field when the Who is = ‘G.’
17.3 Intellect prints the payments on the days' Journals, displays them in the patient ledger, and sends an email that includes a report and a receipt.
18. Primary/Sec/All 
18.1 Effective version 16.02.22. This field is used to write off balances. See Payment --► Auto Payment --►Write-Off Balance.
18.2 Effective version 16.10.11, an 'All' option was added to the drop-down list. 'All' is now the default.
19. When the information is completely entered, select one of these options:
19.1 [Commit/Exit] allows an 'Automatic Payment Journal' to be produced when these conditions match posted claims: 1. Patient Account Number, 2. DOS, 3. CPT Code, 4. Modifier, and 5. Charge Amount.
Click [Commit/Exit] to display the Print Automatic Payment dialog box:
19.1.1.1 Printer: The default printer for the logged-in clinic and password is selected. To select a different printer, either click on the arrow, OR press the → (right arrow) on the keyboard to view the list of printer codes. In our example, the defaulted Printer is HP. This is just an example of a printer name and may or may not be set up on the system.
To select the printer type, click on the code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
An Intellect Noridian Set Up video tutorial is available on our website at www.primeclinical.com. Select [Onstaff/Intellect Info], and then [Intellect Noridian Set Up]. Note: Log-in to see the video. Current support is required.
19.1.1.2 Number of Copies: This field defaults to either 0 (zero) or 1. Both print 1 copy. To print more than one copy, enter the number of copies.
19.1.2 Fax/Email:
In addition to printing reports, Intellect provides the capability to export reports to an Excel spreadsheet, Email, Fax, Disk, or Archive. A secondary printer may also be selected, if one is set up, by clicking on the arrow to display the drop-down list.
19.1.3 Select the [Print] button to send your request to the printer (or as a Fax or email).
19.1.4 Select the [Cancel] button to clear the screen and return to the Auto Payment screen without saving or printing.
19.2 Click [Cancel/Exit] to display this prompt:
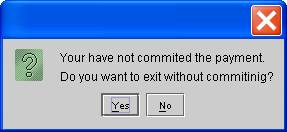
19.2.1 Click [No] to commit and exit.
19.2.2 Click [Yes] to exit without committing.
Automatic Payment Journal, and 'Error Report'
After clicking on [Commit/Exit], Intellect produces an 'Automatic Payment Journal' when these conditions match posted claims: 1. Patient Account Number, 2. DOS, 3. CPT Code, 4. Modifier, and 5. Charge Amount. The 'Automatic Payment Journal' lists all payments and adjustments posted.
Effective version 9.12.10 - Modification: Automatic Payment Journal report header/fields
These changes were made to the Automatic Payment Journal report:
* The Deductible column was moved to the left
* The Patient’s Name is only listed once
* In the ACN column the HIC number is only shown once
* The code in the Check/CCN column now displays as it comes from the insurance company and is only listed once
When the program is unable to match records in the ERA file to posted claims, Intellect produces a second report; i.e., an 'Error Report' (see below). The records on the 'Error Report' need to be posted manually.

Effective version 13.03.01: As of this update, unapplied credits or debits on the ERA that comes from the payer now display on both the Automatic Payment Journal report and Error Report (see above). These items could include a loan repayment, a capitation payment, a partial refund, etc. The report displays 'Unapplied Credit' whether or not the amount is a credit or debit.
Note: Per the ANSI 835, use the PLB segment to allow adjustments that are NOT specific to a particular claim or service to the amount of the actual payment. These adjustments can either decrease the payment (a positive number) or increase the payment (a negative number). Some examples of PLB adjustments are a loan repayment or a capitation payment. Multiple adjustments can be placed in one PLB segment, grouped by the provider identified in PLB01 and the period identified in PLB02. Although the PLB reference numbers are not standardized, refer to the HCFA Medicare Part A and B instructions for code suggestions and usage guidelines.
1539 Example: PLB]123456]19960930]CV:9876514]-1.27~
The system was unable to post the records shown on the 'Error Report', therefore, they need to be posted manually.
NOTE 1:
• Intellect allows clients to determine which ERA Reason Codes should be applied during Auto Posting and which should not. See the documentation on Utility --► Message --► Reason Codes.
• If posting a Secondary insurance segment with Reason Code 42 and Qualifier CO, the system does not apply the adjustment.
• Intellect ALWAYS posts the payment regardless of the set up of the Reason Codes table.
• The Reason Codes table set up applies to only the Deductible and Adjustment segments.
• The descriptions of the Reason Codes have been added to the bottom of the Automatic Payment Journal.

NOTE 2: When posting primary insurance payments through the Payment --► Auto Payment feature and the primary insurance denied the claim, Intellect sets the ‘Approved’ amount to $0.00. The ‘Approved’ amount is a required element in the electronic claim record when billing the secondary insurance.