
Intellect™
MANAGEMENT MENU OPTIONS

Detail
Detail Report
The Detail screen provides management with approximately 25 different reports allowing analysis of charges, payments, and adjustments as returned and viewed by various operational perspectives. Information may be requested based on ICD, procedure codes, date range, provider, category, gender, age, facility, provider department, referring, or insurance. Some reports display aging. Some analyze percentages. Detail Reports display requested information as it was at the time of posting the charge.
With this Management Report, Intellect provides the capability to print, export to Email or Fax, or to an Excel spreadsheet.
Note: When reports are exported to Excel, all of the information is grouped together in all the reports except the Diagnosis Report, Summary Diagnosis Report, and Deleted Charge Report. By contrast, in Intellect, some reports separate the information by a provider (e.g., clinic, provider, etc.). For example, in Intellect, the Detail Procedure by Provider report has a page break and subtotals between each Provider's information and has a heading identifying the Provider for whom the report is generated. In Excel, the Detail Procedure by Provider report does not have identifying headers nor does it have a break or subtotals between Providers.
Note: For all Management reports, the patient's Category and Insurance at the time of posting from the Charge screen is associated with that item forever.
Display the Print Detail screen.
Updates:
Effective version 19.01.18, the Name of the Report in the report header coincides with the <Report Code> drop-down selection:

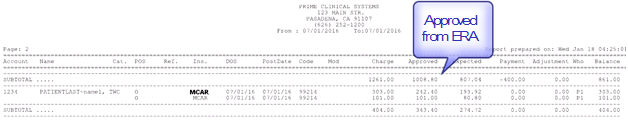
Software versions previous to 17.02.17 included the approved amounts from the Fee Schedule in all the Management Detail reports. Effective version 17.02.17, if payment was posted via an Automatic ERA file and the approved amount from the Payer was included in the ERA file, Intellect updates the th_actual approved when the amount is greater than zero and prints this on the Detail Report. If the th_actual approved is not populated in the ERA file then Intellect updates the th_approved from the fee schedule if one exists.
For example:
Utility/Procedure/Fee Schedule
Detail Report Sample for CPT 99214
Effective Version 12.12.06. In the past, in columns such as Expected, Payment, Adjustment, etc., if an entry had no monetary value, the column would be blank. As of version 12.12.06, if an entry has no monetary value, Intellect displays 0.00 in the column.
Effective Version 9.12.18, a few of the report codes (including the first 5 of them) print sub totals based on the sort field, if any is chosen. Additionally, some reports may also be exported to Excel. Please go to Reports Programmed for Excel Import for more information.
1. To display the Print Detail Screen in Intellect, go to Management --► Detail
The Print DETAIL_MAIN screen displays:

Effective Version 9.12.10 Field Modification. The one- and two-character code choices on the drop-down lists have been replaced with explanatory choices, making the code selection more user-friendly and comprehensive.
Note: The drop-down list descriptions for the code choices have remained the same, allowing correlation between the old and new code choices.
2. Report Code 
2.1 Use the drop-down list to select the type of report. There is no default and a selection must be made. Press the [F2] search key to display the valid choices:
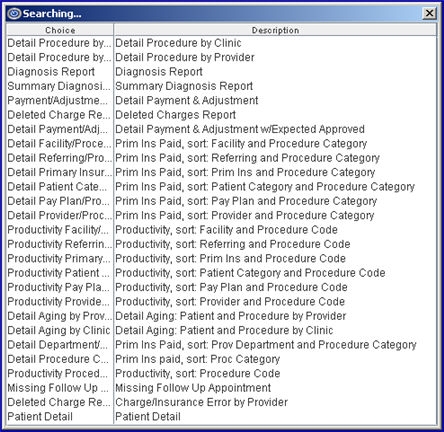
2.2 Version 9.12.09 Modification. In this version, the former single-character code choices on the drop-down list were replaced with complete word choices to make the code selection easier. In the brief summaries of each Detail Report which follow, the former single-character code choice appears in parenthesis behind the new Report Code choice.
2.3 Detail Procedure by Clinic (C): The Detail Procedure Report gives Patient Account Number, Name, Category, Place of Service, Referring, Insurance, Date of Service, Posting Date, Code, Modifier, Charge, Approved, Payment, Expected Payment Adjustment, Who, and Balance of Charges. These are a few benefits:
2.3.1 The report could list patients who had charges entered for that day, totaling those charges as well as any payments posted that day towards those charges.
2.3.2 The report could provide a list of patients whose balance is still due from their secondary insurance companies based on a specified last payment date.
2.3.3 The report could provide information for a specific procedure noting the approved, payment, adjustment, and charge amount(s) sorting this by insurance.
2.3.4 The report could provide a report for all charges still on 'Hold' status (Ledger --► Accounting or Ledger --►Open Item <W> (Who column) still equals 'Y').
To request this report, review the information for the remaining fields on this screen and populate them as applicable.
2.4 Detail Procedure by Provider (A): This is the same information as in 'Detail Procedure by Clinic (C)' except it is grouped and totaled by Provider.
2.5 Diagnosis Report (D): This report looks at the Diagnosis Entry Date and compares it to the Charge Entry Date. The Diagnosis Report gives Patient Account Number, Name, Category, Phone, Date of Service, ICD10 Code, and Description and is followed by the Summary Diagnosis Report. It may be requested for a specific provider, category, gender, age from and to range, CPT Code, ICD10 Code (e.g., 949.5, or by using the asterisk, 94*, to include all ICD10 codes that begin with '94'), facility, insurance, or referring. The date selection for this report is always the entry date. These are a few benefits:
2.5.1 The report could list all patients with the specified ICD10, insurance, and CPT Code in order to correct an incorrect ICD10 and rebill.
2.5.2 The report could list all patients with a certain diagnosis for patients between a set of ages and to facilitate a drug rep with a new drug.
2.5.3 The report could list all patients with a certain diagnosis so they can be informed of a new laser technique to correct a condition.
To request this report, review the information for the remaining fields on this screen and populate them as applicable.
2.6 Summary Diagnosis Report (S): The Summary Diagnosis Report displays each diagnosis code used during the specified date range, and a count of how many times the diagnosis code was used. The Group number (if available) and description of the code are included.
2.7 Payment/Adjustment Report (P): Detail Payments and Adjustments for patients. All fields apply to this report. This report uses only the first set of dates. The program pulls ALL the charges based on the payment date.
2.8 Deleted Charge Report (X): Deleted Charges Report.
2.9 Detail Payment/Adjustment Report (J): Detail Payments and Adjustments for patients with Approved and Expected. All fields apply to this report. This report uses only the first set of dates. The program pulls ALL the charges based on the payment date.
Effective version 16.11.10, the Detail Payment and Adjustment report now includes a ‘User’ column. This column displays the User # of the user who posted the charge/adjustment.
Effective version 17.06.09, changes were made to a portion of this report:
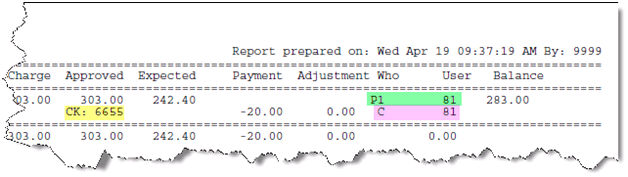
• The yellow highlighted area now displays the check number for the payment. The check number can be up to 16-characters in length, and is pulled from either Charges --►Charge <Payment>, or any of the payment options in the Payment Menu when the check number is included as part of the transaction.
• As a point of reference, the green highlighted area indicates the responsible party for the Who at the time the charge was posted, and the user who posted the charge.
• The pink highlighted area above indicates who is now responsible for the balance of the charge after the payment was made.
2.10 Detail Facility/Procedure Category (2): Primary Insurance vs. Other Payments, subtotaled by Facility Code and sorted by Procedure Category.
2.11 Detail Referring/Procedure Category (3): Primary Insurance vs. Other Payments, subtotaled by Referring Code and sorted by Procedure Category.
2.12 Detail Primary Insurance/Procedure Category (6): Primary Insurance vs. Other Payments, subtotaled by primary Insurance Code and sorted by Procedure Category.
2.13 Detail Patient Category/Procedure Category (5): Primary Insurance vs. Other Payments, subtotaled by Patient Category Code and sorted by Procedure Category.
2.14 Detail Pay Plan/Procedure Category (4): Primary Insurance vs. Other Payments, subtotaled by Pay Plan Code and sorted by Procedure Category.
2.15 Detail Provider/Procedure Category (7): Primary Insurance vs. Other Payments, subtotaled by Provider Code and sorted by Procedure Category.
2.16 Productivity Facility/Procedure Category (W): Primary Insurance vs. Other Payments, subtotaled by Facility Code and sorted by Procedure Code.
2.17 Productivity Referring/Procedure Category (B): Primary Insurance vs. Other Payments, subtotaled by Referring Code and sorted by Procedure Code.
2.18 Productivity Primary Insurance/Procedure Category (H): Primary Insurance vs. Other Payments, subtotaled by primary Insurance Code and sorted by Procedure Code.
2.19 Productivity Patient Category/Procedure Category (G): Primary Insurance vs. Other Payments, subtotaled by Patient Category Code and sorted by Procedure Code.
2.20 Productivity Pay Plan/Procedure Category (E): Primary Insurance vs. Other Payments, subtotaled by Pay Plan Code and sorted by Procedure Code.
2.21 Productivity Provider/Procedure Category (O): Primary Insurance vs. Other Payments, subtotaled by Provider Code and sorted by Procedure Code.
2.22 Detail Aging by Provider ("+"): Detail Aging Balance, returned by Provider listed by Patient. Version 9.12.14 - New Columns. To provide more information, three columns were added to the Detail Aging by Provider and Detail Aging by Clinic reports. The columns are Who, PINS (Primary Insurance Code), SINS (Secondary Insurance Code), and Cat (Category).
2.23 Detail Aging by Clinic ("-"): Detail Aging Balance detail Procedure for the Clinic, sorted by Patient. Version 9.12.14 - New Columns. To provide more information, three columns were added to the Detail Aging by Provider and Detail Aging by Clinic reports. The columns are Who, PINS (Primary Insurance Code), SINS (Secondary Insurance Code), and Cat (Category).
2.24 Detail Department/Procedure Category (8): Primary Insurance vs. Other Payments, subtotaled by Provider Department Code and sorted by Procedure Category.
2.25 Detail Procedure Category (9): Primary Insurance vs. Other Payments, subtotaled by Procedure Category and sorted by Procedure Category.
2.26 Productivity Procedure Code (Z): Primary Insurance vs. Other Payments, subtotaled by Procedure Category and sorted by Procedure Category.
2.27 Missing Follow Up Appointment (M): This report pulls patients and their Category, Home Phone, Work Phone, and Cell Phone numbers from the Patient Registration screen. The criteria for inclusion are a charged procedure that has no follow up appointment scheduled.
2.28 Detail Charge Report (N): Charge/Insurance error by Provider. This report compares the charged insurance(s) P1, S1, etc. to the patient's current insurance set up and displays if there are any discrepancies. The report is organized by provider.
2.29 Patient Detail Effective Version 12.12.06: This report displays both a section and a subtotal for each patient.
2.30 PQRS (Quality Reporting) Effective Version 16.02.22: The Physician Quality Reporting System (PQRS) is a quality reporting program that encourages individual eligible professionals (EPs) and group practices to report information on the quality of care to Medicare. For additional information on PQRS, see PQRS Billing Requirements 2016.
The PRQS/Quality report generated by Intellect may not be printed directly. Instead, it allows Medicare information to be saved to an Excel format via the Print Dialog Box by selecting EXCEL from the <Printer> field drop-down list, naming it as specified by the requester, and subssequently saving it where desired.
The PQRS report includes information in these columns: TIN (tax ID number), NPI, HIC (Health Insurance Card number), First Name, Last Name, Patient Account, Patient Gender, Patient date of birth (DOB), Visit Date, Prime Insurer, Secondary Insurer, ICD, CPT, Modifier, and place of service (POS).
When generating this report, please note:
• ONLY the following fields may be applied: <Provider>, <Billing Provider>, <From Date>/<To> (only the first <From Date>/<To> date range should be used in this report, as this report only takes into consideration the charge dates ), <Gender>, <Category>, <Age From/To>, <Code C>, <Facility>, <Referring>, <Department>, <Who>, <Date Selection>, <Modifier>, and <Zip Code> fields.
• In order for the HIC field on the PQRS report to be filled with the subscriber ID, the patient's insurance on the Registration screen must match the insurance on the Charge screen, and the insurance coverage date must be equal to or prior to the charge date; in other words, the date of service (DOS) must be after the coverage 'From' date.
Note: The PQRS report is always based on the billing provider's individual NPI, regardless of what options are entered when requesting the report.
2.31 Benchmarking Report Effective version 16.05.20: This report shows the cost effectiveness of procedures performed by an individual provider only if the supplies used for specific procedure codes and the cost of each supply are entered in the Utility --► Procedure --► Supply --►Add screen.
3. From Date 
3.1 There are two sets of dates that perform different selection criteria dependent on the Report code selected. These dates work together to determine the return results. This is the beginning date of the first set. The first set of dates is required and defaults to the current system date.
3.2 If Report Code 'Detail Procedure by Clinic (C)' is selected, then these dates identify the entry, service, last payment, or first billing date of the charges as determined by the <Date Selection> field entry.
3.3 If Report Codes 'Detail Procedure by Clinic (D)' and 'Summary Diagnosis Report (S)' are selected, then these dates define the entry date(s) of the requested information. Remember to enter a wide range of entry dates. The second set of dates defines the time period.
3.4 The beginning date is as follows:
3.4.1 Report Code Detail Procedure by Clinic (C):
If a date for a procedure based on the <Date Selection> field criteria falls within the range established by the first To Date and From Date, then the procedure's charge (and accompanying information) are included on the report.
3.4.2 Report Codes Diagnosis Report (D) and Summary Diagnosis Report (S):
These dates define the entry date(s) of the requested information. They are always based on the entry date(s) of the charges associated with the requested diagnosis (<Date Selection> must always be E).
4. To 
4.1 The ending date to include in the first date range as described above.
4.2 The first set of dates is required and defaults to the current system date.
5. Provider 
5.1 Leave blank for the default of all providers for all Report Code types.
5.2 To filter the results based on a specific provider, type the Utility --► Provider --► Provider <Provider Code>.
5.3 This field does NOT accept multiple values, but accepts the asterisk * to return all Providers starting with the portion of the code entered prior to the *. For example, J* prints all Providers whose code begins with J.

6.1 Leave blank for the default of all providers for all Report Code types.
6.2 To filter the results based on a specific provider, type the Utility --► Provider --► Provider <Provider Code>.
6.3 This field accepts multiple values:
• provider codes separated by commas with no space:
• a range of codes entered with a hyphen and no spaces:

• an asterisk * to return all providers starting with the portion of the code entered prior to the *. For example, 1* prints all providers whose code begins with 1.
7. Date From 
7.1 This is the beginning date of the second set of <Date From> and <Date To>.
7.2 <Date From><To>, when used, generates ALL PAYMENTS entered for the selected time frame.
7.3 For Report Code Detail Procedure by Clinic (C):
7.3.1 If the procedure returned in the first date range has payment(s), and or adjustment(s) that fall in the range established by the second <To Date> and <From Date> entries, they are displayed on the report. This always uses the entry date of payments and adjustments.
7.3.2 If left blank, all payment(s), and/or adjustment(s) for the procedures returned in the first date range are displayed on the report
7.4 For Report Codes Diagnosis Report (D) and Summary Diagnosis Report (S):
7.4.1 Entries define the service date(s) of ONLY those charges selected as a result of the first set of dates, associated with the requested diagnosis.
7.4.2 When more than one date of service is posted during the same charge session, only the first charge date is displayed on the report.
7.5 For Report Code Detail Payment & Adjustment (P), leave blank.
8. To 
8.1 The ending date to include in the second date range as described above.
8.2 Payment and adjustment detail, per charge, is ONLY displayed on the report when dates are entered in the second set of date fields.
8.3 For Report Code Detail Payment & Adjustment (P), leave blank.
9.1 No specific gender is the default for all Report Code types (leave blank).
9.2 To filter the results based on a specific gender, use the drop-down to select Male, Female, or Unknown if the gender is unknown or not applicable (e.g., Company Accounts).
9.3 When requesting the Diagnosis Report, if <Gender> and <Diagnosis> are populated on this screen, Intellect ONLY looks at the <Gender> in Registration --►Patient and not the Utility --►Diagnosis <Gender> (which is ONLY for Charge posting to trigger a pop-up when the patient's gender and procedure code do not match).
10. Category 
10.1 Leave blank for the default of all categories for all Report Code types.
10.2 To request the report for a specific category, type the Utility --► Category <Category Code>.
10.3 This field accepts multiple values:
• separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Categories starting with the portion of the code entered prior to the *. For example, M* prints all Categories whose code begins with M.
10.4 The report includes this information based on the category assigned to the patient at the time of posting charges, which at the time of running the report may not be the patient's current category.
11.1 This is the youngest age in whole years to filter the results by age. It is determined by patient age at date of service (DOS). For example, if the youngest age to include in the report is one, enter 01.
11.2 For the default of including all ages for all Report Code types, leave this field blank.
11.3 Note for PQRS reports: The fields <Age From> and <Age To> require the year of the patient's birth to be entered as a 2-digit number. For example, to request a report for patients born in the range of 1995 to 1998, enter 95 in the <Age From> field and enter 98 in the <Age To> field.
12. Age To 
12.1 This is the maximum age in whole years to filter the results by age determined by patient age at date of service (DOS). For example, if the oldest age to include in the report is ninety-five, enter 95.
12.2 For the default of including all ages for all Report Code types, leave this field blank.
12.3 Note for PQRS reports: The fields <Age From> and <Age To> require the year of the patient's birth to be entered as a 2-digit number. For example, to request a report for patients born in the range of 1995 to 1998, enter 95 in the <Age From> field and enter 98 in the <Age To> field.
13. Code C 
13.1 Leave blank for the default of all posted codes for all Report Code types.
13.2 To request the report for a specific code, type the Utility --► Procedure --► Procedure <Code C>.
13.3 This field accepts multiple values:
• separated by commas with no spaces:

• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Procedures starting with the portion of the code entered prior to the *. For example, 9* prints all Procedures whose code begins with 9.
13.4 In most cases, Utility --► Procedure --► Procedure <Code C> is the field used for CPT Coding. Whether this is true in your case or not, the report looks to this field ONLY for its Panel Code criteria. Keep in mind, procedures with HCPCs (usually entered on Code E) and X codes (usually entered on Code R) need to have the Code C value entered on this field in order for this to be captured in the report. To print a procedure listing, use Procedure --► Print as it lists Codes R, C, and E.
14. Procedure Category 
14.1 Leave blank for the default of all procedure categories for all Report Code types.
14.2 To request the report for a specific procedure category, type the Utility --► Procedure --► Procedure <Category>.
15.1 This field is used with the Diagnosis Report (D) to return a report with results for only patients whose posted charge contains the specified diagnosis.
15.2 Enter the Utility --► Diagnosis <Diagnosis Code> to request the report for only one diagnosis.
15.3 To return a report with results for patients whose posted charge contains a diagnosis series, the asterisk (*) may be used in requesting the criteria. For example, to request a report for each Utility --► Diagnosis <Diagnosis Code> within the 940 series, enter 94*. The * is not used with the Summary Diagnosis Report (S) Report Code.
15.4 This field accepts multiple values:
• separated by commas with no spaces:

• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Diagnoses starting with the portion of the code entered prior to the *. For example, 9* prints all Diagnoses whose code begins with 9.
15.5 Enter the value found in the Utility --► Diagnosis <Diagnosis Code> field, NOT the actual diagnosis code found in the Utility --► Diagnosis <ICD9/ICD10 Code> field. Although the Diagnosis Report (D) and Summary Diagnosis Report (S) are requested by the Utility --► Diagnosis <Diagnosis Code>, the report displays the <ICD9/ICD10 Code> field. In most cases, both field values are the same with the exception of speed-coded diagnoses on a Superbill.
15.6 When requesting the Diagnosis Report, if <Gender> and <Diagnosis> are populated on this screen, Intellect ONLY looks at the <Gender> in Registration --►Patient and not the Utility --►Diagnosis <Gender>.
16. Diagnosis Group 
16.1 This field is used only with the Report Codes Diagnosis Report (D) and Summary Diagnosis Report (S).
16.2 To request the report for a specific diagnosis group, type the Utility --► Diagnosis --► Diagnosis <Group>.
17. Facility 
17.1 Leave blank for the default of all facilities for all Report Code types.
17.2 To request the report for a specific facility, type the Utility --►Facility <Facility Code>.
17.3 This field accepts multiple values:
• separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:

• an asterisk * to return all Facilities starting with the portion of the code entered prior to the *. For example, 1* prints all Facilities whose code begins with 1.
18. Insurance 
18.1 Leave blank for the default of all primary insurers for all Report Code types.
18.2 To request the report for a specific primary insurer, type the Utility --► Insurance --► Insurance <Insurance Co Code>.
18.3 This field accepts multiple values:
• separated by commas with no spaces:
• an asterisk * to return all Insurers starting with the portion of the code entered prior to the *. For example, M* prints all Insurers whose code begins with M.
19. Referring 
19.1 Leave blank for the default of all referrals for all Report Code types.
19.2 To request the report for a specific referral source, type the Utility --► Referring <Referring Code>.
19.3 This field accepts multiple values:
• separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Referrers starting with the portion of the code entered prior to the *. For example, 1* prints all Referrers whose code begins with 1.
20. Employer Code 
20.1 Effective version 14.12.30 - New field.
20.2 Leave blank for the default of all employers/companies for all <Report Code> types.
20.3 To request the report for a specific employer/company, type the Utility --►Business <Company Code>.
20.4 This field accepts multiple values:
• separated by commas with no spaces:
• an asterisk * to return all employers/companies starting with the portion of the <Company Code> entered prior to the *. For example, A* prints all employers/companies whose <Company Code> begins with A.

20.5 Via this field, Intellect can also pull data based on the employer attached to the Charges. For the employer to attach to any charges, this information must be set up in Intellect:
Patient --►Registration <Employer Name>
Patient --►Worker --►Worker Insurance <Employer>.
21. Department 
21.1 Leave blank for the default of all departments for all Report Code types.
21.2 To request the report for a specific department, type the Utility --► Provider --► Provider <Department> name or number.
21.3 This field currently does NOT accept multiple values or a department range.
22.1 This field is used only for the Detail Procedure by Clinic (C) Report Code.
22.2 This field defaults to the Utility --► Set Up --► Parameter <Date Selection> field entry (usually Entry Date). Note: <Date Selection> is an optional field and may not be on the screen. To have this field, please contact PCS support.
22.3 Accept this default OR use the drop-down list to select the desired option.
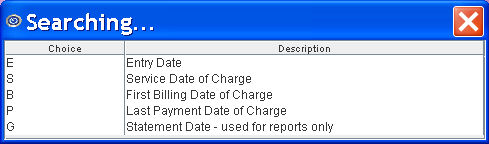
22.4 Click on the field, OR press the [F2] key to display the valid choices
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
All versions prior to 9.12.10

23.1 This field is used for Report Codes Detail Procedure by Clinic (C), Detail Procedure by Provider (A), Detail Payment & Adjustment (P), Detail Aging by Provider (+), Detail Aging by Clinic ( -), and Detail Payment/Adjustment Report (J).
23.2 This field defaults to All Charges (formerly A). Additional options include: unpaid charges, charges with a positive balance, charges with a negative balance, charges with any balance other than zero, or only charges with a zero balance.
23.3 Accept the default OR use the drop-down list to make an alternate selection.
23.4 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10

All versions prior to 9.12.10

24. Billed 
24.1 This field is used only for the Detail Procedure by Clinic (C) Report Code.
24.2 This field defaults to All Charges (formerly A). Other options allow a report to be requested for either billed charges or only unbilled charges.
24.3 Accept the default OR use the drop-down list to make an alternate selection.
24.4 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
All versions prior to 9.12.10

25. Who 
25.1 This field is used only for the Detail Procedure by Clinic (C) Report Code.
25.2 The default is blank, not filtering by the Ledger --► Accounting or Ledger --►Open Item <Who> column.
25.3 Accept this default OR use the drop-down list to filter by the selected 'W' type.
25.4 Accept the blank default OR use the drop-down list to filter by the selected Who type. Partial lists are shown below:
Effective after 9.12.10:
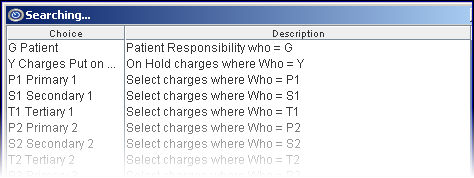
Effective 9.12.10:

26. Date Selection 
26.1 This field defaults to Entry Date for the Detail Procedure by Clinic (C) Report Code.
26.2 Accept the default OR use the drop-down to make an alternate selection.
26.3 For the Diagnosis Report (D) Report Code, it is recommended to accept the default.
26.4 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
All versions prior to 9.12.10
27. FileName 
27.1 Not available at this time.
28. Modifier 
28.1 This field is used only for <Report Code> Detail Procedure by Clinic (C).
28.2 Leave blank to return a report that includes all modifiers.
28.3 To filter the results by specific modifier, type in the Utility --►Procedure --►Modifier <Modifier Code>.
29. Zip Code 
29.1 Enter the appropriate zip code.
29.2 This optional field is used to limit the report based on the home address <Zip Code> on the patient’s Registration screen.
30. Adjustment Code 
30.1 Effective Version 12.12.06
30.2 This field is used in conjunction with the Detail Payment/Adjustment Report.
30.3 Enter any Utility --►Messages --►Remark <Remark Code> used to define the source of adjustment when posting adjustments.
31. Payment Code 
31.1 Effective Version 12.12.06
31.2 This field is used in conjunction with the Detail Payment/Adjustment Report.
31.3 Enter any Utility --►Messages --►Remark <Remark Code> used to define the source of payment when posting payments.
32. When the information is completely entered, select one of these options:

32.1 Click [Print] OR press [Enter] to display the Print Remittance (Detail Report) dialog box:
32.1.1 Printer Properties:
32.1.1.1 Printer: The default printer for the logged-in clinic and password is selected. To select a different printer, either click on the arrow, OR press the → (right arrow) on the keyboard to view the list of printer codes. In our example, the defaulted Printer is HP. This is just an example of a printer name and may or may not be set up on the system.
To select the printer type, click on the code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code; then press the [Enter] key to select.
32.1.1.2 Number of Copies: This field defaults to either 0 (zero) or 1. Both print 1 copy. To print more than one copy, enter the number of copies.
32.1.2 Fax/Email:
In addition to printing reports, Intellect provides the capability to export reports to an Excel spreadsheet, Email, Fax, Disk, or Archive. A secondary printer may also be selected, if one is set up, by clicking on the arrow to display the drop-down list.
32.1.3 Select the [Print] button to send the request to the printer (or as a Fax or email).
32.1.4 Select the [Cancel] button to clear the screen and return to the Print DETAIL_MAIN screen without saving or printing.
32.2 Click [Clear] to clear all information and return the focus to the <Report Code> field without saving.
32.3 Click [Exit] to clear the screen and return the focus to the main Intellect screen.
SAMPLE MANAGEMENT DETAIL REPORTS